Valid Texas Do Not Resuscitate Order Template
In the realm of healthcare decisions, the Texas Do Not Resuscitate (DNR) Order form stands as a vital tool for individuals wishing to express their preferences regarding life-sustaining treatments. This document allows patients to communicate their wishes about resuscitation efforts in the event of a medical emergency, ensuring that their desires are respected by healthcare providers. It is essential for patients to understand that the DNR form is not just a piece of paper; it carries significant implications for end-of-life care. By completing this form, individuals can specify that they do not want cardiopulmonary resuscitation (CPR) or other advanced life-saving measures in situations where their heart stops or they stop breathing. The form must be signed by both the patient and a physician, affirming that the decision has been made thoughtfully and in accordance with the patient's medical condition. Furthermore, this order is not only applicable in hospitals but also extends to other healthcare settings, such as nursing homes and at-home care, making it a crucial aspect of personal healthcare planning. Understanding the nuances of the Texas DNR Order form empowers individuals to take control of their healthcare decisions and ensures their values and wishes are honored when it matters most.
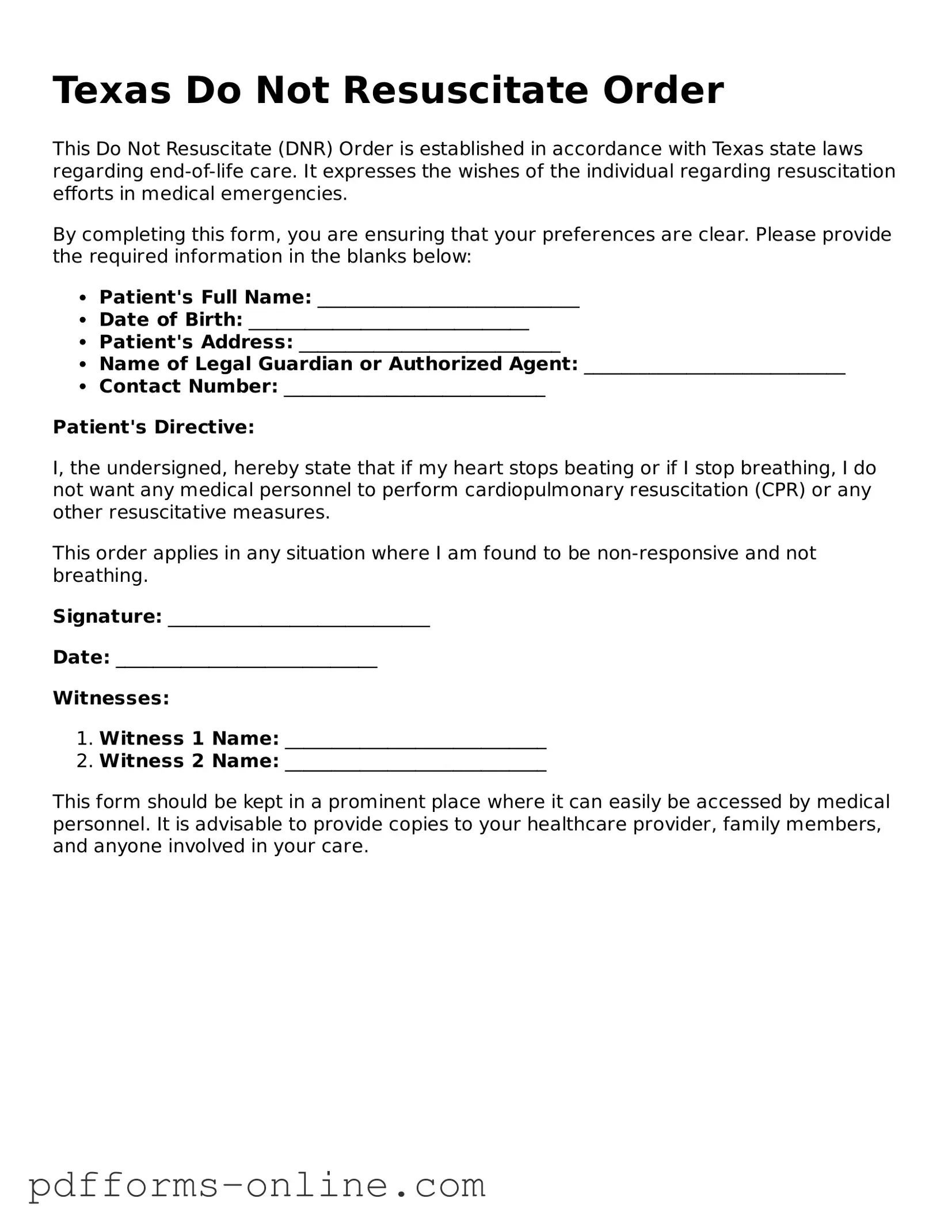
Document Example
Texas Do Not Resuscitate Order
This Do Not Resuscitate (DNR) Order is established in accordance with Texas state laws regarding end-of-life care. It expresses the wishes of the individual regarding resuscitation efforts in medical emergencies.
By completing this form, you are ensuring that your preferences are clear. Please provide the required information in the blanks below:
- Patient's Full Name: ____________________________
- Date of Birth: ______________________________
- Patient's Address: ____________________________
- Name of Legal Guardian or Authorized Agent: ____________________________
- Contact Number: ____________________________
Patient's Directive:
I, the undersigned, hereby state that if my heart stops beating or if I stop breathing, I do not want any medical personnel to perform cardiopulmonary resuscitation (CPR) or any other resuscitative measures.
This order applies in any situation where I am found to be non-responsive and not breathing.
Signature: ____________________________
Date: ____________________________
Witnesses:
- Witness 1 Name: ____________________________
- Witness 2 Name: ____________________________
This form should be kept in a prominent place where it can easily be accessed by medical personnel. It is advisable to provide copies to your healthcare provider, family members, and anyone involved in your care.
Frequently Asked Questions
-
What is a Do Not Resuscitate (DNR) Order in Texas?
A Do Not Resuscitate Order is a legal document that instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) if a patient’s heart stops beating or if they stop breathing. In Texas, this order is recognized by healthcare providers and is an important part of end-of-life care planning.
-
Who can request a DNR Order?
A DNR Order can be requested by a patient who is of sound mind and understands the implications. If the patient is unable to make decisions, a legally authorized representative, such as a family member or healthcare proxy, may request the order on their behalf.
-
How do I obtain a DNR Order form in Texas?
You can obtain a DNR Order form from various sources, including hospitals, healthcare providers, and online resources. The Texas Department of State Health Services provides a standardized DNR form that is widely accepted. Ensure that the form is properly filled out and signed.
-
What information is required on the DNR Order form?
The form typically requires the patient’s name, date of birth, and the signature of the patient or their authorized representative. It must also be signed by a physician who agrees with the decision to issue a DNR Order.
-
Is a DNR Order valid outside of a hospital?
Yes, a DNR Order is valid in various settings, including at home, nursing homes, and other healthcare facilities. It is essential to ensure that the order is clearly visible and accessible to emergency medical personnel.
-
Can I change or revoke a DNR Order?
A DNR Order can be changed or revoked at any time. The patient or their authorized representative should communicate this decision to their healthcare provider and ensure that the updated order is documented properly.
-
What happens if a DNR Order is not followed?
If a DNR Order is not followed, it may lead to legal consequences for the medical personnel involved. However, it is crucial that the order is clearly documented and available to avoid confusion during emergencies.
-
How does a DNR Order affect other medical treatments?
A DNR Order specifically addresses resuscitation efforts. It does not affect other medical treatments or interventions. Patients can still receive pain relief, comfort care, and other necessary medical treatments as outlined in their care plan.
-
Can I discuss my DNR Order with my healthcare provider?
Yes, discussing your DNR Order with your healthcare provider is highly encouraged. They can provide guidance, answer questions, and help ensure that your wishes are documented and respected in your medical care.
Misconceptions
Understanding the Texas Do Not Resuscitate (DNR) Order form is crucial for making informed healthcare decisions. Here are six common misconceptions surrounding this important document:
- A DNR order means no medical care will be provided. This is incorrect. A DNR order specifically instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. Other medical treatments and interventions can still be administered.
- Only terminally ill patients can have a DNR order. This misconception is false. While many individuals with terminal illnesses choose to complete a DNR order, anyone can request one based on their personal healthcare preferences, regardless of their current health status.
- A DNR order is permanent and cannot be changed. This is misleading. A DNR order can be revoked or modified at any time by the patient or their legally authorized representative. It is important to communicate any changes to healthcare providers.
- Family members can decide on a DNR order without the patient's consent. This is not accurate. A DNR order must be based on the patient's wishes. Family members can discuss preferences, but the final decision should come from the patient or their authorized representative.
- Having a DNR order means you will not receive any life-saving measures. This is a misunderstanding. A DNR order only applies to CPR. Other life-saving measures, such as medications or treatments for other medical conditions, can still be administered.
- Once a DNR is signed, it is automatically recognized everywhere. This is incorrect. While a DNR order is valid in Texas, its recognition may vary in other states or facilities. It is advisable to check local regulations and ensure that the DNR order is properly documented and communicated.
Common mistakes
-
Not Including Required Signatures: One common mistake is failing to secure all necessary signatures. The form must be signed by both the patient and their physician. Without these signatures, the order may not be honored.
-
Incorrect Patient Information: Providing inaccurate or incomplete information about the patient can lead to confusion. Ensure that the patient's full name, date of birth, and other identifying details are correct.
-
Misunderstanding the Scope of the Order: Some individuals do not fully grasp what a Do Not Resuscitate (DNR) order entails. It is crucial to understand that this order specifically addresses resuscitation efforts and does not affect other medical treatments.
-
Failure to Discuss with Family: Not discussing the DNR order with family members can lead to misunderstandings and emotional distress. Open communication is essential to ensure everyone is on the same page regarding the patient’s wishes.
-
Not Updating the Order: Life circumstances and medical conditions can change. Failing to update the DNR order when necessary can result in unwanted interventions. Regular reviews of the document are advisable.
-
Using an Outdated Form: Using an old version of the DNR form can cause complications. Always ensure that the most current version is being utilized, as laws and regulations may have changed.
-
Ignoring State-Specific Requirements: Each state may have unique requirements for DNR orders. Ignoring Texas-specific regulations can render the order invalid. Familiarize yourself with local laws to ensure compliance.
Find Some Other Do Not Resuscitate Order Forms for Specific States
Pennsylvania Dnr - It’s advisable to discuss DNR options with your healthcare provider for guidance.
When engaging in a vehicle sale in Ohio, it is essential to utilize the Ohio Motor Vehicle Bill of Sale to ensure a smooth transfer of ownership. This document not only serves as proof of the transaction but also includes critical details regarding the vehicle and the seller and buyer involved. For a comprehensive understanding of how to complete this form, you can refer to the resource available at https://documentonline.org/blank-ohio-motor-vehicle-bill-of-sale, which provides valuable insights and guidance.
Dnr Form Nc - Family members are encouraged to understand their loved one’s wishes related to a DNR to avoid confusion during crises.
PDF Attributes
| Fact Name | Description |
|---|---|
| Definition | The Texas Do Not Resuscitate (DNR) Order is a legal document that allows individuals to refuse resuscitation in the event of a medical emergency. |
| Governing Law | This form is governed by Texas Health and Safety Code, Chapter 166. |
| Eligibility | Any adult can create a DNR order, provided they are competent to make healthcare decisions. |
| Signature Requirements | The DNR order must be signed by the patient or their legally authorized representative, along with a physician's signature. |
| Form Availability | The DNR order form can be obtained from healthcare providers, hospitals, or online from the Texas Department of State Health Services. |
| Revocation | A DNR order can be revoked at any time by the patient or their representative, verbally or in writing. |
| Emergency Medical Services | Emergency medical personnel must honor a valid DNR order when responding to a medical emergency. |
| Limitations | The DNR order only applies to resuscitation efforts and does not affect other medical treatments or care. |
Similar forms
The Texas Do Not Resuscitate Order (DNR) form is similar to an Advance Directive. An Advance Directive is a legal document that allows individuals to outline their healthcare preferences in case they become unable to communicate those wishes. Like the DNR, it provides guidance to healthcare providers about the individual's desires regarding medical treatment. Both documents aim to ensure that a person's wishes are respected, particularly in critical situations where they may not be able to speak for themselves.
Another document comparable to the DNR is a Living Will. A Living Will specifies what types of medical treatment an individual wants or does not want in situations where they are terminally ill or permanently unconscious. Similar to the DNR, it focuses on end-of-life care and allows individuals to express their wishes clearly. Both documents serve to communicate preferences to healthcare providers and family members, helping to avoid confusion during difficult times.
For those looking to secure a place to live, understanding the Florida Rental Application process is pivotal. This document, crucial for tenant evaluation, provides insights into a potential renter's background and financial standing. To learn more, visit the important Florida Rental Application form guidelines.
The Medical Power of Attorney (MPOA) also shares similarities with the DNR form. An MPOA designates a specific person to make healthcare decisions on someone’s behalf if they are unable to do so. While the DNR focuses specifically on resuscitation efforts, the MPOA covers a broader range of medical decisions. Both documents empower individuals to ensure their healthcare preferences are honored, either through direct instructions or by appointing a trusted person to make those decisions.
Lastly, the Physician Orders for Life-Sustaining Treatment (POLST) form is another document akin to the DNR. The POLST form translates a patient’s wishes regarding life-sustaining treatments into actionable medical orders. Like the DNR, it is intended for individuals with serious health conditions and aims to ensure that their preferences are followed in emergency situations. Both forms are designed to communicate critical healthcare decisions clearly and effectively to medical personnel, ensuring that patient autonomy is respected.