Blank Tb Test Template
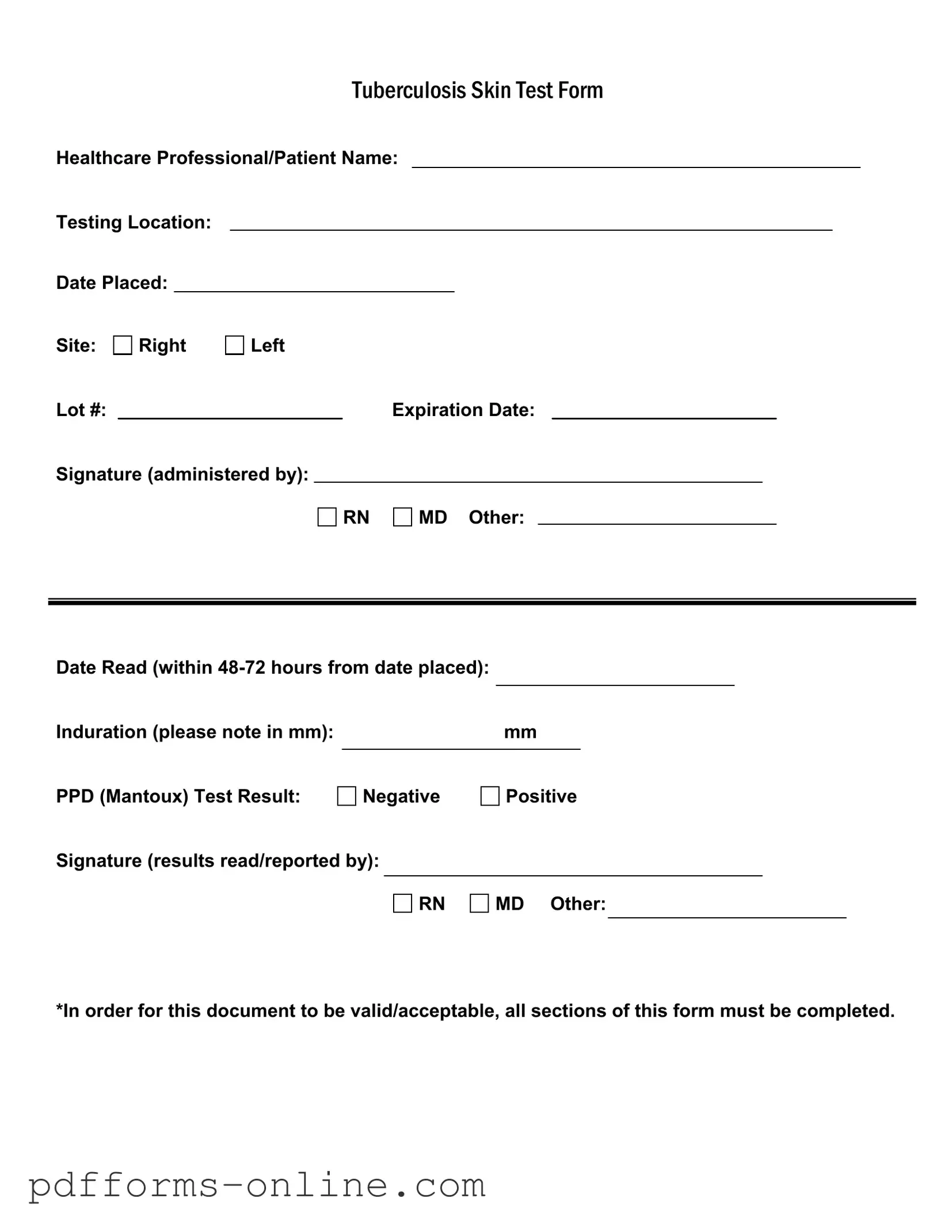
The Tuberculosis (TB) Skin Test Form is a crucial document used in the assessment and monitoring of tuberculosis exposure. It captures essential information about the healthcare professional administering the test, as well as the patient receiving it. Key details include the names of both the healthcare provider and patient, the location where the test is conducted, and the date the test was placed. The form also specifies the site of administration, indicating whether it was on the right or left arm. Important identifiers such as the lot number and expiration date of the test materials ensure validity. The signature of the administering professional—whether a registered nurse (RN), medical doctor (MD), or other qualified personnel—confirms the test's administration. Additionally, the form requires a follow-up reading within 48 to 72 hours, noting the induration measurement in millimeters and the PPD (Mantoux) test result, which indicates whether the test was negative or positive. A final signature from the professional who reads and reports the results adds an extra layer of verification. It is vital that all sections of this form are completed for it to be considered valid and acceptable in medical settings.
Document Example
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Frequently Asked Questions
-
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. This form ensures that all necessary information is recorded for both healthcare professionals and patients, facilitating accurate tracking and reporting of TB test results.
-
What information is required on the TB Test form?
To ensure the document is valid, all sections must be completed. This includes:
- Healthcare Professional/Patient Name
- Testing Location
- Date Placed
- Site of the test (Right or Left)
- Lot number and expiration date of the test
- Signature of the person administering the test (RN, MD, or Other)
- Date Read (which should be within 48-72 hours from the date placed)
- Induration measurement in mm
- PPD Test Result (Negative or Positive)
- Signature of the person reading/reported the results (RN, MD, or Other)
-
How soon should the results be read?
The results of the TB test should be read within 48 to 72 hours after the test is administered. This timeframe is crucial for accurately measuring the induration, which is the raised area at the test site.
-
What does the induration measurement indicate?
Induration is measured in millimeters (mm) and indicates the body's immune response to the TB test. A higher induration measurement typically suggests a positive result, meaning that the individual may have been exposed to the TB bacteria. Specific thresholds for positive results can vary based on individual risk factors.
-
What do the test results mean?
The PPD test results can be either Negative or Positive:
- A Negative result indicates that there is no evidence of TB infection.
- A Positive result suggests that the individual may have been exposed to TB, and further evaluation may be necessary.
-
Who is qualified to administer and read the TB Test?
The TB test must be administered and read by qualified healthcare professionals, such as a registered nurse (RN) or a medical doctor (MD). Their signatures are required on the form to validate the test process.
-
What happens if the TB Test form is incomplete?
If any sections of the TB Test form are left incomplete, the document may be considered invalid or unacceptable. This could lead to issues in tracking results or in follow-up care, making it essential to ensure that every part of the form is filled out accurately.
Misconceptions
Understanding the Tuberculosis (TB) Test form can be challenging. Here are ten common misconceptions that people often have about this form:
- The TB Test form is only for healthcare professionals. Many individuals may need to fill out the form themselves or provide information, especially if they are undergoing testing for employment or school requirements.
- Only a doctor can administer the TB test. While doctors can administer the test, registered nurses (RNs) and other qualified healthcare professionals can also perform this task.
- The expiration date of the test is irrelevant. The expiration date is crucial, as using a test that has expired can lead to inaccurate results.
- A negative result means no exposure to TB. A negative result indicates no active TB disease, but it does not rule out past exposure or latent TB infection.
- The form does not require a signature. A signature from the administering healthcare professional is necessary for the form to be valid.
- Induration measurement is optional. Induration measurement is essential; it helps determine the test result's significance and must be documented.
- The test can be read at any time after placement. The test must be read within 48-72 hours after placement to ensure accurate results.
- Only positive results need to be reported. Both negative and positive results must be documented and reported on the form.
- The site of the test placement is not important. Noting the site (right or left arm) is important for record-keeping and follow-up purposes.
- Completing the form is optional. All sections of the form must be completed for it to be valid and acceptable.
Being informed about these misconceptions can help ensure that the TB testing process goes smoothly and that all necessary information is accurately documented.
Common mistakes
-
Incomplete Personal Information: Failing to fill in the healthcare professional or patient name can lead to confusion and delays.
-
Missing Testing Location: Not specifying where the test was conducted can complicate record-keeping.
-
Incorrect Date Placed: Writing the wrong date can affect the timeline for reading the results.
-
Site Selection Errors: Indicating the wrong site (right or left arm) can lead to inaccuracies in testing.
-
Lot Number Omission: Forgetting to include the lot number can render the test invalid.
-
Expiration Date Not Noted: Leaving the expiration date blank can raise questions about the test's validity.
-
Signature Absence: Not signing where the test was administered can cause issues with verification.
-
Missing Date Read: Failing to document the date the results were read can lead to confusion.
-
Induration Measurement Errors: Not recording the induration correctly in millimeters can lead to incorrect interpretations.
-
Test Result Misreporting: Incorrectly marking the PPD test result as negative or positive can lead to serious health implications.
Additional PDF Templates
Prehospital Medical Care Directive - Completing the directive can foster better communication among family about health care decisions.
For those seeking a move-in ready home, obtaining the right Florida Rental Application can streamline your application process, allowing landlords to efficiently assess your suitability as a tenant. You can access the necessary form through this key Florida Rental Application resource for guidance.
Bdsm Limit List - Interest in discussing safe words and consent protocols.
Broward Animal Care and Adoption - Include any notes regarding allergies or adverse reactions to vaccines.
Document Data
| Fact Name | Description |
|---|---|
| Form Purpose | This form is used to document the results of a Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. |
| Healthcare Professional | The form requires the name of the healthcare professional administering the test, which could be an RN (Registered Nurse), MD (Medical Doctor), or other qualified personnel. |
| Testing Location | It is important to specify the location where the TB test is administered for record-keeping and accountability. |
| Date Placed | The form must include the date the test was placed, which is crucial for determining when the results should be read. |
| Induration Measurement | Results are noted in millimeters (mm) of induration, which is the raised area at the test site. This measurement helps determine the test outcome. |
| Result Interpretation | The test result can be either negative or positive, indicating whether or not the individual has been exposed to TB. |
| Signature Requirement | Both the administering professional and the individual reading the results must sign the form to validate the findings. |
| Completion Requirement | To be valid, all sections of the form must be fully completed. Incomplete forms may not be accepted. |
Similar forms
The Tuberculosis (TB) Test form bears similarities to the Immunization Record. Both documents serve as official proof of a person's health status regarding infectious diseases. The Immunization Record lists vaccinations received, including dates and types, much like the TB Test form details the testing process and results. Each document requires signatures from healthcare professionals to validate the information, ensuring accountability and reliability in health records.
Another document akin to the TB Test form is the Medical Clearance Form. This form is often used in various settings, such as employment or school admissions, to confirm that an individual is free from communicable diseases. Similar to the TB Test form, it requires specific details about the individual’s health status, the healthcare provider’s information, and a signature. Both documents aim to ensure public safety by confirming that individuals do not pose a health risk to others.
The Health History Questionnaire also shares characteristics with the TB Test form. It collects essential information about a person's medical background and potential exposure to illnesses. While the TB Test form focuses on a specific test result, the Health History Questionnaire provides a broader overview of health, including past conditions and vaccinations. Both documents are crucial in assessing an individual’s health and determining any necessary follow-up actions.
In addition to various medical forms, businesses utilize legal documents such as the Non-compete Agreement to safeguard their interests. This agreement ensures that employees do not engage in activities that could harm the business's competitive position, paralleling how medical forms protect patient information and safety. For those in Arizona wishing to draft a Non-compete Agreement, it is advisable to reference All Arizona Forms to ensure compliance and effectiveness.
The Release of Information form is another document that bears resemblance to the TB Test form. This form allows healthcare providers to share a patient’s health information with other entities, such as employers or schools. Like the TB Test form, it requires a signature from the patient to authorize the release, ensuring that sensitive health information is handled appropriately and with consent.
The Patient Consent Form is similar as well, as it is used to obtain permission from patients before any medical procedure or test is performed. Just like the TB Test form, it outlines the specifics of what the patient is consenting to, ensuring they understand the implications of the test. Both documents emphasize the importance of informed consent in healthcare, protecting the rights of patients while facilitating necessary medical actions.
The Fitness for Duty form also parallels the TB Test form. This document assesses an employee’s ability to perform their job safely and effectively, often requiring medical evaluations. Similar to the TB Test form, it includes information about health assessments, signatures from healthcare professionals, and is often time-sensitive. Both forms play a vital role in ensuring that individuals are fit to engage in activities that could impact their health or the health of others.
The School Health Assessment form is another comparable document. This form is often required for student enrollment and includes health screenings, immunizations, and assessments for communicable diseases. Much like the TB Test form, it ensures that children are healthy and ready to attend school, providing necessary information to schools for maintaining a safe environment for all students.
The Pre-Employment Health Screening form shares similarities as well. This document is utilized by employers to assess the health status of potential hires, often including tests for communicable diseases. Like the TB Test form, it requires detailed information about the individual's health and the signature of a healthcare provider, ensuring that the information is accurate and trustworthy for employment decisions.
Lastly, the Occupational Health Assessment form is similar to the TB Test form. This document evaluates employees’ health in relation to their specific job duties, often focusing on exposure to workplace hazards. Both forms require detailed health information and professional signatures, emphasizing the importance of maintaining a healthy workforce while protecting both employees and the public.