Valid Ohio Do Not Resuscitate Order Template
The Ohio Do Not Resuscitate (DNR) Order form serves as a crucial document for individuals who wish to communicate their preferences regarding medical interventions in the event of a life-threatening situation. This form is designed to guide healthcare providers in respecting a patient’s wishes about resuscitation efforts, particularly in cases where a patient may be unable to articulate their desires due to medical conditions. It is important to note that the DNR Order is specific to cardiopulmonary resuscitation (CPR) and does not encompass other medical treatments. The form must be completed and signed by a physician, ensuring that it reflects the informed consent of the patient or their legal representative. Additionally, it is essential for the form to be easily accessible to healthcare professionals at all times, especially in emergency situations. Ohio law mandates that the DNR Order be honored across various healthcare settings, including hospitals, nursing homes, and home care environments. Understanding the implications of this form is vital for patients and their families as they navigate end-of-life care decisions, emphasizing the importance of clear communication between patients and their healthcare providers.
Document Example
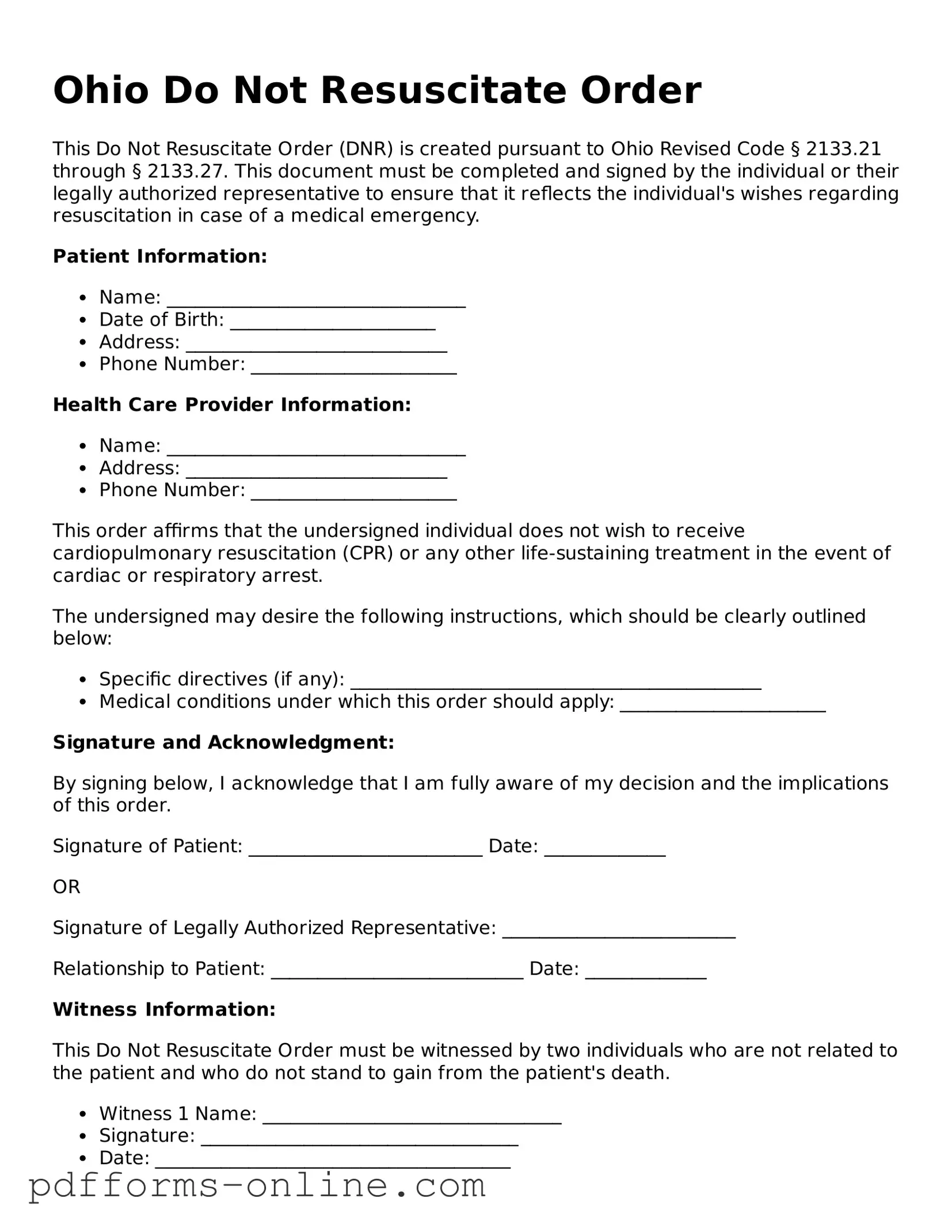
Ohio Do Not Resuscitate Order
This Do Not Resuscitate Order (DNR) is created pursuant to Ohio Revised Code § 2133.21 through § 2133.27. This document must be completed and signed by the individual or their legally authorized representative to ensure that it reflects the individual's wishes regarding resuscitation in case of a medical emergency.
Patient Information:
- Name: ________________________________
- Date of Birth: ______________________
- Address: ____________________________
- Phone Number: ______________________
Health Care Provider Information:
- Name: ________________________________
- Address: ____________________________
- Phone Number: ______________________
This order affirms that the undersigned individual does not wish to receive cardiopulmonary resuscitation (CPR) or any other life-sustaining treatment in the event of cardiac or respiratory arrest.
The undersigned may desire the following instructions, which should be clearly outlined below:
- Specific directives (if any): ____________________________________________
- Medical conditions under which this order should apply: ______________________
Signature and Acknowledgment:
By signing below, I acknowledge that I am fully aware of my decision and the implications of this order.
Signature of Patient: _________________________ Date: _____________
OR
Signature of Legally Authorized Representative: _________________________
Relationship to Patient: ___________________________ Date: _____________
Witness Information:
This Do Not Resuscitate Order must be witnessed by two individuals who are not related to the patient and who do not stand to gain from the patient's death.
- Witness 1 Name: ________________________________
- Signature: __________________________________
- Date: ______________________________________
- Witness 2 Name: ________________________________
- Signature: __________________________________
- Date: ______________________________________
It is advisable that copies of this order be shared with all healthcare providers and kept in accessible locations to ensure compliance with the patient's wishes.
Frequently Asked Questions
-
What is a Do Not Resuscitate (DNR) Order in Ohio?
A Do Not Resuscitate Order is a medical directive that informs healthcare providers not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest or respiratory failure. In Ohio, this order is legally recognized and must be followed by medical personnel. The intent is to respect the wishes of individuals who do not wish to undergo resuscitation efforts, which may prolong suffering or conflict with their personal beliefs about end-of-life care.
-
Who can request a DNR Order?
In Ohio, a DNR Order can be requested by any competent adult who understands the implications of the order. Additionally, a parent or legal guardian can request a DNR for a minor. It is crucial that the individual requesting the DNR has the capacity to make informed decisions regarding their medical care. In cases where a person is unable to make decisions for themselves, a legally appointed representative may be able to request a DNR on their behalf.
-
How is a DNR Order completed in Ohio?
To complete a DNR Order in Ohio, a specific form must be filled out and signed. This form includes sections for the patient’s information, the signature of the patient or their representative, and the signature of a physician. It is important to ensure that the form is properly completed and that copies are distributed to relevant healthcare providers, including hospitals and emergency medical services. The DNR Order should be kept in an easily accessible location, such as with the patient’s medical records or at home.
-
Is a DNR Order valid outside of a hospital setting?
Yes, a DNR Order is valid outside of a hospital setting in Ohio, provided that it is properly executed and recognized by emergency medical personnel. This means that if a person with a DNR Order experiences a medical emergency outside of a hospital, first responders must adhere to the order. It is advisable for individuals with a DNR to carry the order with them or wear a medical alert bracelet that indicates their wishes regarding resuscitation.
-
Can a DNR Order be revoked?
Absolutely. A DNR Order can be revoked at any time by the individual who signed it or their legal representative. This can be done verbally or in writing, but it is best to document the revocation to avoid any confusion. Healthcare providers should be notified immediately of any changes to ensure that the patient’s current wishes are respected.
-
What should individuals discuss with their healthcare providers regarding a DNR Order?
Individuals considering a DNR Order should have open and honest discussions with their healthcare providers. Topics may include the patient’s overall health status, prognosis, and the potential outcomes of resuscitation efforts. Understanding the implications of a DNR Order is essential. It is also beneficial to discuss other advance care planning options, such as living wills or healthcare proxies, to ensure comprehensive end-of-life care preferences are documented.
Misconceptions
Understanding the Ohio Do Not Resuscitate (DNR) Order form can be challenging. Here are five common misconceptions that people may have:
-
Anyone can fill out a DNR form.
Only a patient or their legally authorized representative can complete the DNR order. This ensures that the decision reflects the patient's wishes.
-
A DNR order means no medical treatment at all.
A DNR order specifically applies to resuscitation efforts during a cardiac or respiratory arrest. Other treatments, such as medications or surgeries, can still be provided.
-
Once a DNR is in place, it cannot be changed.
A DNR order can be revoked or modified at any time by the patient or their representative. It’s important to communicate any changes to healthcare providers.
-
All healthcare providers automatically know about a DNR order.
It is crucial to ensure that the DNR order is easily accessible and communicated to all healthcare professionals involved in the patient’s care.
-
A DNR order is only for terminally ill patients.
A DNR order can be appropriate for anyone who wishes to avoid resuscitation, regardless of their health status. It reflects personal choices about end-of-life care.
Common mistakes
-
Not Including Required Information: Individuals often forget to provide essential details, such as the patient's name, date of birth, and the signature of the physician. Missing this information can render the form invalid.
-
Failure to Discuss with Healthcare Providers: Some people fill out the form without consulting their healthcare team. This can lead to misunderstandings about the patient's medical condition and preferences.
-
Inaccurate or Ambiguous Language: Using vague terms or unclear instructions can cause confusion. It is crucial to state the patient's wishes clearly to avoid misinterpretation.
-
Not Updating the Form: Life circumstances change. Failing to update the Do Not Resuscitate Order after significant health changes or shifts in personal wishes can lead to unintended consequences.
-
Neglecting to Inform Family Members: Some individuals do not communicate their decision to family members. This can lead to conflict or distress during critical moments when the order is needed.
-
Not Understanding Legal Implications: People may not fully grasp the legal weight of the Do Not Resuscitate Order. It is important to understand how it fits into broader healthcare and legal frameworks.
Find Some Other Do Not Resuscitate Order Forms for Specific States
Do Not Resuscitate Form Michigan - Family members can sometimes serve as authorized representatives to complete the DNR for another person.
Illinois Do Not Resuscitate - It is crucial to discuss your DNR preferences with your healthcare provider for comprehensive understanding.
Can You Have a Dnr at Any Age - Supports patient autonomy in the face of medical emergencies.
To ensure a smooth transaction and comply with state regulations, it is essential to have the appropriate documentation when buying or selling a trailer in Florida. The Florida Trailer Bill of Sale form captures all necessary details regarding the sale, including the date of sale, purchase price, and the trailer's specifications. For your convenience, click here to get the form to facilitate this important process.
Do Not Resuscitate Order - Creating a DNR can provide clarity and reduce stress for family members during critical situations.
PDF Attributes
| Fact Name | Description |
|---|---|
| Definition | The Ohio Do Not Resuscitate (DNR) Order form allows individuals to refuse resuscitation efforts in case of cardiac or respiratory arrest. |
| Governing Law | This form is governed by Ohio Revised Code Section 2133.21, which outlines the legal framework for DNR orders in the state. |
| Eligibility | Any adult who is capable of making informed decisions about their medical care can complete a DNR order. |
| Required Signatures | The form must be signed by the patient or their legal representative, along with a physician's signature to be valid. |
| Distribution | It is essential to provide copies of the DNR order to healthcare providers and family members to ensure adherence to the patient's wishes. |
Similar forms
The Ohio Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive, which is a broader legal document that outlines a person's preferences for medical treatment in the event they are unable to communicate their wishes. Like the DNR, an Advance Directive can specify a person's desire to forego resuscitation and other life-sustaining treatments. Both documents require the individual’s signature and, in some cases, the signatures of witnesses or a notary, ensuring that the person’s wishes are respected in critical medical situations.
Another document akin to the DNR is the Physician Orders for Life-Sustaining Treatment (POLST). This form is designed for patients with serious illnesses and translates their treatment preferences into actionable medical orders. Similar to the DNR, the POLST form must be signed by a physician and is intended to be honored by healthcare providers. Both documents serve to communicate a patient’s wishes regarding resuscitation and other life-sustaining measures, but the POLST offers a more comprehensive approach to medical treatment preferences.
The Georgia Trailer Bill of Sale form is essential not only for providing legal clarity in trailer transactions but also for ensuring that all parties involved are aware of their rights and responsibilities. This document serves as a testament to the sale, detailing information such as the purchase price and specific characteristics of the trailer being sold. For those looking to obtain or create a Trailer Bill of Sale, resources like onlinelawdocs.com/ can be invaluable in navigating the legal requirements efficiently.
The Living Will is another document that aligns closely with the DNR Order. A Living Will allows individuals to express their wishes regarding end-of-life care and the use of life-sustaining treatments. While a DNR specifically addresses resuscitation efforts, a Living Will encompasses a broader range of medical interventions. Both documents provide critical guidance to healthcare providers and family members, ensuring that a person's healthcare preferences are followed when they cannot voice them themselves.
Health Care Power of Attorney (HCPOA) is yet another related document. This legal instrument designates an individual to make medical decisions on behalf of someone else if they become incapacitated. While the DNR specifies a particular medical intervention, the HCPOA allows the appointed person to make decisions based on the patient's wishes, which may include refusing resuscitation. Both documents work in tandem to ensure that a person’s healthcare preferences are respected.
The Medical Order for Life-Sustaining Treatment (MOLST) also bears resemblance to the DNR Order. Like the POLST, the MOLST is designed to be a medical order that translates a patient’s preferences into actionable directives for healthcare providers. Both documents are intended for individuals with serious health conditions and emphasize the importance of honoring patient autonomy in medical decision-making. They require signatures from healthcare professionals, ensuring that the orders are valid and enforceable.
Lastly, the Do Not Intubate (DNI) order is similar to the DNR in that it specifically addresses a patient's wishes regarding certain medical interventions. A DNI order indicates that a patient does not want to be placed on a ventilator or have intubation performed in the event of respiratory failure. While the DNR focuses on resuscitation efforts, both documents serve to communicate critical healthcare preferences to medical staff, thereby ensuring that a patient’s wishes are honored in urgent situations.