Valid North Carolina Do Not Resuscitate Order Template
In North Carolina, the Do Not Resuscitate (DNR) Order form plays a crucial role in ensuring that individuals receive care aligned with their wishes in critical medical situations. This legally binding document allows patients to express their preference regarding resuscitation efforts in the event of a cardiac arrest or respiratory failure. It is designed for individuals who, after careful consideration and discussion with their healthcare providers, choose not to undergo CPR or other life-saving measures. The form must be completed and signed by a physician, and it is essential for patients to share copies with their family members and healthcare team to ensure that their wishes are known and respected. Understanding the implications of a DNR order is vital, as it can significantly affect the course of medical treatment and end-of-life care. Additionally, the form includes specific guidelines about its use, ensuring clarity for both patients and medical professionals. By taking the time to understand and complete a DNR order, individuals can empower themselves and their loved ones to make informed decisions about their healthcare preferences during some of life’s most challenging moments.
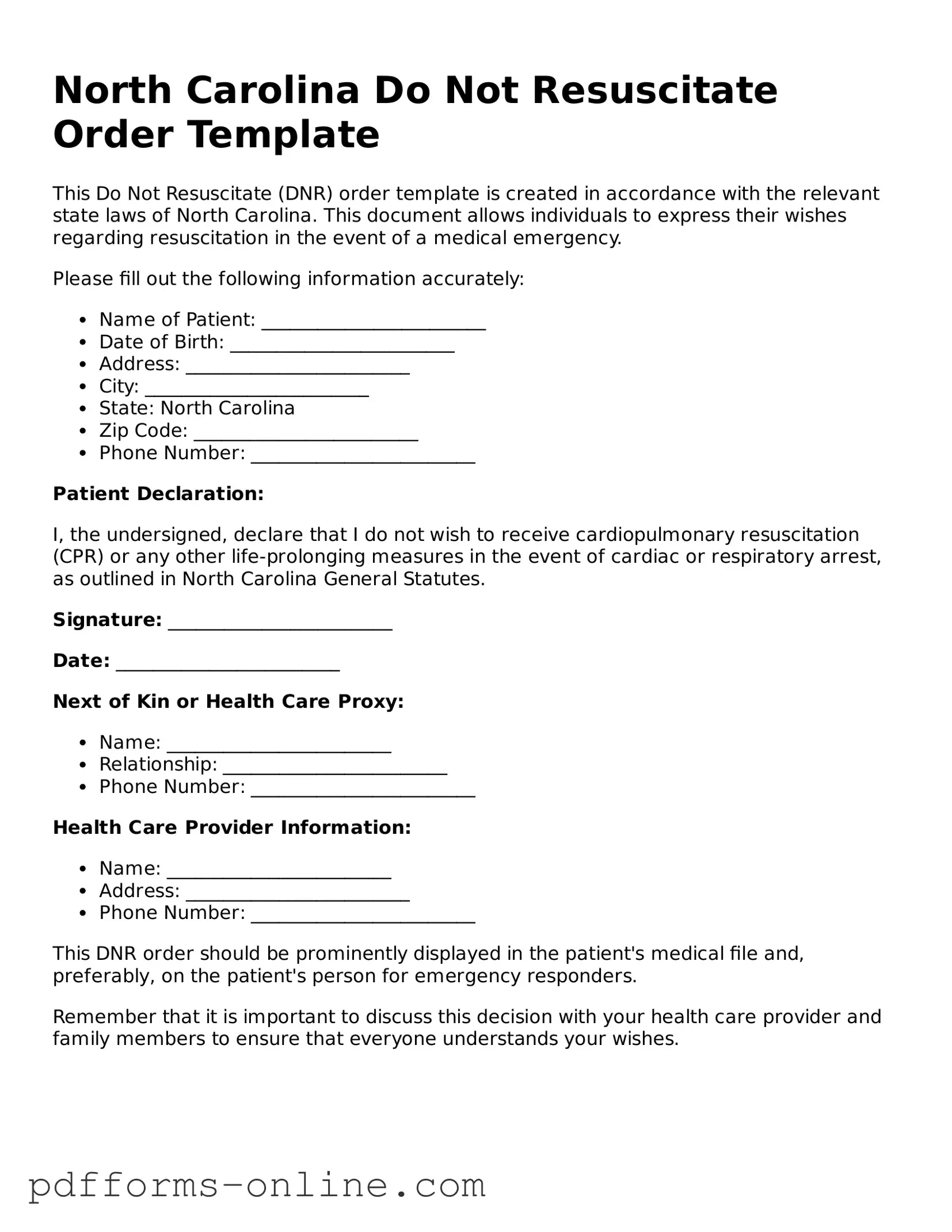
Document Example
North Carolina Do Not Resuscitate Order Template
This Do Not Resuscitate (DNR) order template is created in accordance with the relevant state laws of North Carolina. This document allows individuals to express their wishes regarding resuscitation in the event of a medical emergency.
Please fill out the following information accurately:
- Name of Patient: ________________________
- Date of Birth: ________________________
- Address: ________________________
- City: ________________________
- State: North Carolina
- Zip Code: ________________________
- Phone Number: ________________________
Patient Declaration:
I, the undersigned, declare that I do not wish to receive cardiopulmonary resuscitation (CPR) or any other life-prolonging measures in the event of cardiac or respiratory arrest, as outlined in North Carolina General Statutes.
Signature: ________________________
Date: ________________________
Next of Kin or Health Care Proxy:
- Name: ________________________
- Relationship: ________________________
- Phone Number: ________________________
Health Care Provider Information:
- Name: ________________________
- Address: ________________________
- Phone Number: ________________________
This DNR order should be prominently displayed in the patient's medical file and, preferably, on the patient's person for emergency responders.
Remember that it is important to discuss this decision with your health care provider and family members to ensure that everyone understands your wishes.
Frequently Asked Questions
-
What is a Do Not Resuscitate (DNR) Order in North Carolina?
A Do Not Resuscitate Order is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. In North Carolina, this order specifically indicates that a person does not want to receive cardiopulmonary resuscitation (CPR) or other life-saving measures if their heart stops beating or they stop breathing.
-
Who can request a DNR Order?
Any adult who is capable of making their own healthcare decisions can request a DNR Order. This includes individuals with terminal illnesses or those who wish to avoid aggressive medical interventions. Additionally, a legal guardian or authorized healthcare proxy can request a DNR on behalf of someone who is unable to make decisions for themselves.
-
How do I obtain a DNR Order in North Carolina?
To obtain a DNR Order, you must complete the official North Carolina DNR Order form. This form can be acquired from healthcare providers, hospitals, or online through the North Carolina Department of Health and Human Services website. Once completed, it must be signed by a physician and the patient or their authorized representative.
-
What should I do with the DNR Order once it is completed?
After completing the DNR Order, keep the original document in a safe but accessible location. It is crucial to provide copies to your healthcare provider, family members, and anyone else involved in your care. You may also want to carry a copy with you, especially when visiting healthcare facilities.
-
Can I change or revoke my DNR Order?
Yes, you can change or revoke your DNR Order at any time. To do this, you must destroy the original document and inform your healthcare providers of your decision. If you choose to create a new DNR Order, it should be completed and signed following the same procedures as the original.
-
Will my DNR Order be honored in all healthcare settings?
In most cases, your DNR Order will be honored in hospitals, nursing homes, and other healthcare settings. However, it is essential to communicate your wishes clearly with your healthcare team. Some facilities may have specific protocols regarding DNR Orders, so discussing your preferences with them is advisable.
-
What happens if I do not have a DNR Order?
If you do not have a DNR Order in place, healthcare providers are required to perform resuscitation efforts if your heart stops or you stop breathing. This may include CPR, defibrillation, and other life-saving measures. If you wish to avoid these interventions, it is crucial to establish a DNR Order.
-
Is a DNR Order the same as an advance directive?
No, a DNR Order is not the same as an advance directive, although they are related. An advance directive is a broader document that outlines your overall healthcare preferences, including decisions about life-sustaining treatment and end-of-life care. A DNR Order specifically addresses resuscitation efforts. You can have both documents in place to ensure your wishes are clear.
Misconceptions
- Misconception 1: A Do Not Resuscitate (DNR) order means that no medical care will be provided.
- Misconception 2: DNR orders are only for terminally ill patients.
- Misconception 3: A DNR order is permanent and cannot be changed.
- Misconception 4: Completing a DNR form is complicated and requires extensive legal knowledge.
- Misconception 5: A DNR order is only valid in hospitals.
This is incorrect. A DNR order specifically addresses resuscitation efforts in the event of cardiac or respiratory arrest. It does not prevent other forms of medical treatment or care.
This is a common misunderstanding. While many individuals with terminal conditions may choose to have a DNR, anyone can request one based on their personal health care preferences and values.
This is false. A DNR order can be revoked or modified at any time by the patient or their legal representative, reflecting changes in their wishes or health status.
In reality, the process is designed to be straightforward. Patients or their representatives can typically fill out the form with guidance from healthcare providers without needing legal expertise.
This is misleading. A DNR order can be valid in various settings, including at home or in long-term care facilities, as long as it is properly documented and recognized by the healthcare providers involved.
Common mistakes
-
Not Understanding the Purpose: Many individuals mistakenly believe that a Do Not Resuscitate (DNR) order means that they will not receive any medical care. This is not the case. A DNR specifically addresses the desire to avoid resuscitation in the event of cardiac or respiratory arrest. It does not prevent other forms of treatment or care.
-
Inadequate Discussion with Healthcare Providers: Some people fill out the DNR form without having a thorough conversation with their doctors. This can lead to misunderstandings about the implications of the order. Engaging in open dialogue with healthcare professionals ensures that individuals fully grasp the consequences of their decision.
-
Improper Completion of the Form: Errors in filling out the DNR form can render it invalid. Common mistakes include missing signatures, incorrect dates, or failing to include the necessary identification information. Each detail is crucial for the order to be honored in an emergency situation.
-
Not Communicating Wishes to Family: After completing the DNR form, individuals often neglect to inform their family members about their decision. Without this communication, loved ones may be unaware of the person's wishes during a critical time, leading to confusion and potential conflict.
Find Some Other Do Not Resuscitate Order Forms for Specific States
Illinois Do Not Resuscitate - By establishing a DNR order, you illustrate your commitment to a preferred end-of-life journey.
The Mobile Home Bill of Sale is an important legal document that not only outlines the terms of the sale but also protects both the buyer and seller during the transfer of ownership. To ensure a smooth transaction and to avoid any ambiguities, it's recommended to reference the documentonline.org/blank-new-york-mobile-home-bill-of-sale/ for further guidance and a sample form that can be used in New York.
How Do You Get a Dnr - Emergency medical personnel are trained to respect valid DNR orders.
PDF Attributes
| Fact Name | Description |
|---|---|
| Definition | The North Carolina Do Not Resuscitate (DNR) Order form allows individuals to refuse resuscitation efforts in case of a medical emergency. |
| Governing Law | This form is governed by North Carolina General Statutes, specifically G.S. 90-321 through G.S. 90-324. |
| Eligibility | Any adult can complete a DNR Order, provided they are capable of making their own medical decisions. |
| Signature Requirement | The form must be signed by the individual or their legal representative, along with a physician's signature. |
| Revocation | A DNR Order can be revoked at any time by the individual or their legal representative, simply by destroying the form. |
Similar forms
The North Carolina Do Not Resuscitate (DNR) Order form shares similarities with a Living Will. A Living Will is a legal document that allows individuals to express their wishes regarding medical treatment in the event they become unable to communicate those wishes themselves. Like a DNR, a Living Will typically addresses end-of-life care and can specify the types of medical interventions one does or does not want. Both documents aim to ensure that a person’s preferences are respected when they are unable to advocate for themselves, providing clarity to healthcare providers and loved ones during difficult times.
Another document akin to the DNR is the Medical Power of Attorney. This document designates a trusted person to make healthcare decisions on behalf of someone who is incapacitated. While the DNR specifically focuses on resuscitation efforts, the Medical Power of Attorney can cover a broader range of medical decisions. Both documents serve to uphold an individual’s healthcare wishes, but the Medical Power of Attorney provides a designated agent who can interpret and act on those wishes in various medical situations.
For those interested in ensuring strong legal protections, it is essential to consider documents like the Georgia Hold Harmless Agreement, which can be explored in more detail at onlinelawdocs.com/. This agreement helps clarify responsibilities and liabilities, providing peace of mind in various situations, including property use or construction projects.
The North Carolina DNR Order is also similar to a Physician Orders for Life-Sustaining Treatment (POLST) form. The POLST form is designed for individuals with serious illnesses and translates their treatment preferences into actionable medical orders. Like the DNR, the POLST form is intended to guide healthcare providers in emergency situations. Both documents ensure that a patient’s desires regarding life-sustaining treatments are honored, but the POLST form often includes a wider range of medical interventions beyond resuscitation.
Lastly, the Advance Directive is another document that shares common ground with the DNR Order. An Advance Directive encompasses both the Living Will and the Medical Power of Attorney, allowing individuals to outline their healthcare preferences and appoint a decision-maker. This comprehensive approach ensures that all aspects of a person’s medical care are addressed, including resuscitation preferences. Like the DNR, the Advance Directive aims to provide guidance during challenging medical situations, ensuring that a person’s wishes are respected and followed.