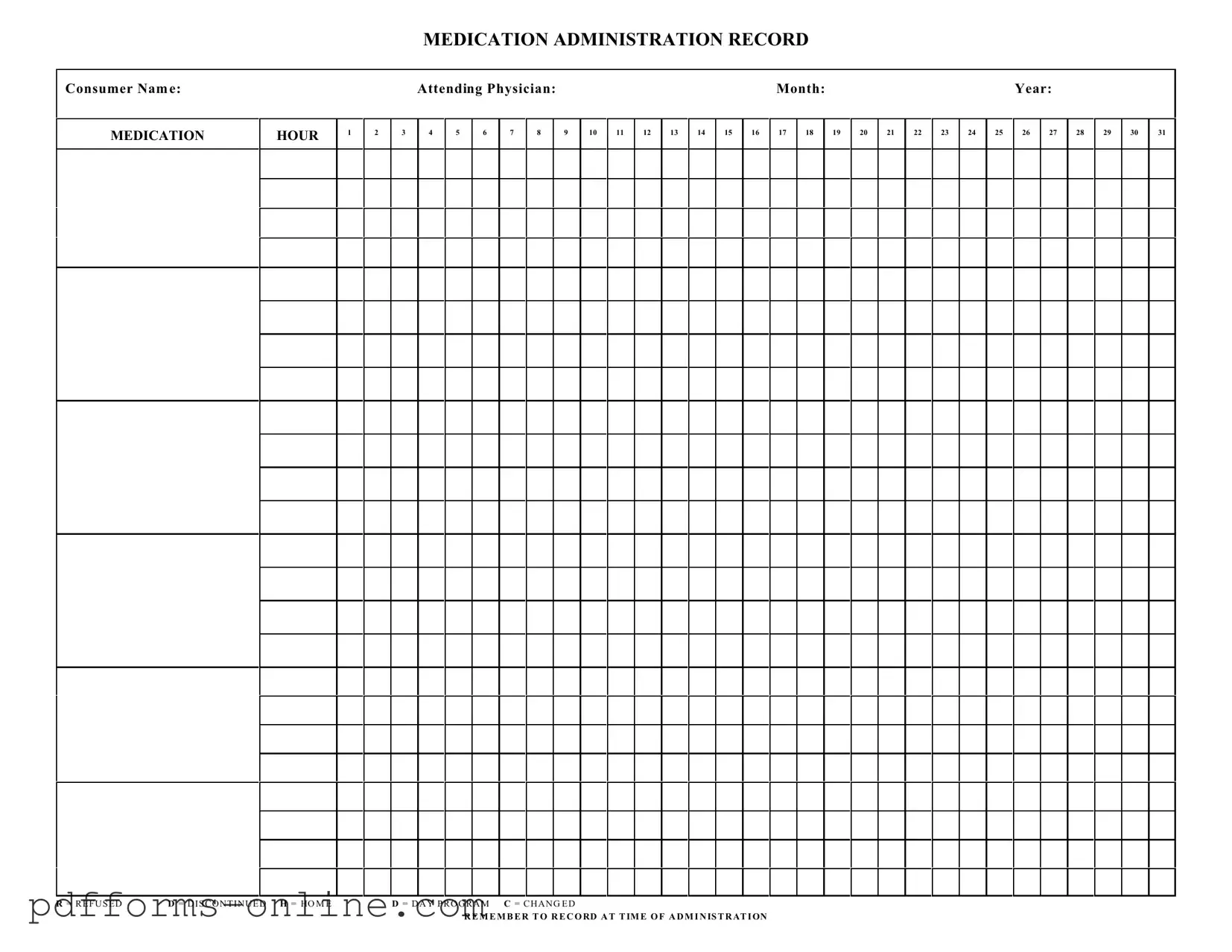
Blank Medication Administration Record Sheet Template
The Medication Administration Record Sheet is an essential tool in healthcare settings, designed to ensure the accurate and timely administration of medications to patients. This form captures crucial information, including the consumer's name and the attending physician, while also detailing the specific medications prescribed. Each day of the month is represented, allowing healthcare providers to track medication administration by hour. Additionally, the form includes vital notations, such as "R" for refused doses, "D" for discontinued medications, and "H" for home administration, which provide clarity on the patient's adherence to their medication regimen. Furthermore, it emphasizes the importance of recording medication administration at the precise time it occurs, thereby fostering accountability and enhancing patient safety. The thoughtful design of this form not only facilitates communication among healthcare professionals but also serves as a critical record that can be reviewed for compliance and care continuity. By maintaining accurate documentation, providers can better understand a patient's medication history, leading to improved health outcomes and more personalized care.
Document Example
MEDICATION ADMINISTRATION RECORD
Consumer Nam e:
MEDICATION
HOUR
1
2
|
Attending Physician: |
|
|
|
|
|
|
|
|
Month: |
|
|
|
|
|
|
|
Year: |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
4 |
5 |
6 |
7 |
8 |
|
9 |
10 |
11 |
12 |
13 |
14 |
15 |
16 |
17 |
18 |
|
19 |
20 |
21 |
22 |
23 |
24 |
25 |
26 |
27 |
28 |
29 |
30 |
31 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
R = R E F U S E D |
D = D I S C O N T I N U E D H = HO M E |
D = D A Y P R O G R A M C = C H A N G E D |
R E M E M B E R T O R E C O RD A T T IM E O F A D M I N IS T R AT I ON
Frequently Asked Questions
-
What is a Medication Administration Record Sheet?
The Medication Administration Record Sheet is a document used to track the administration of medications to individuals. It helps ensure that medications are given at the correct times and in the correct dosages. This form is essential for maintaining accurate records of a patient’s medication regimen.
-
Who should use this form?
This form is typically used by healthcare providers, caregivers, and nursing staff responsible for administering medications. It is designed for use in various settings, including hospitals, nursing homes, and home care environments.
-
How do I fill out the form?
Begin by entering the consumer's name, the attending physician's name, and the month and year at the top of the form. Next, record the medication name and the specific hours at which the medication should be administered. Make sure to note any changes, refusals, or discontinued medications in the appropriate columns.
-
What do the abbreviations R, D, H, M, and C mean?
These abbreviations indicate the status of the medication administration:
- R = Refused
- D = Discontinued
- H = Home
- M = Day Program
- C = Changed
-
Why is it important to record medication administration times?
Recording the exact time of medication administration is crucial for ensuring that patients receive their medications as prescribed. It helps healthcare providers monitor the effectiveness of the medication and identify any potential issues, such as missed doses or adverse reactions.
-
What should I do if a medication is refused?
If a patient refuses medication, mark the appropriate column with an "R" and document the reason for refusal if possible. This information is vital for healthcare providers to understand the patient’s compliance and to make necessary adjustments to their treatment plan.
-
How can I ensure accuracy when using this form?
To ensure accuracy, double-check the medication name, dosage, and administration times before recording. Additionally, have another staff member verify the information when possible. Consistent training and adherence to protocols can also help maintain accuracy.
-
Is this form required by law?
While the specific requirements can vary by state and facility, maintaining accurate medication administration records is generally a legal requirement in healthcare settings. Always check local regulations and facility policies to ensure compliance.
-
Can this form be used for multiple medications?
Yes, the Medication Administration Record Sheet can be used to track multiple medications for a single consumer. Each medication should be recorded in the designated space, ensuring that all relevant information is captured for each one.
Misconceptions
Here are five common misconceptions about the Medication Administration Record Sheet form:
- It’s only for nurses to use. Many people think that only nurses can fill out this form. In reality, anyone involved in administering medication can use it. This includes caregivers and other healthcare professionals.
- It’s not important to keep it updated. Some believe that once the form is filled out, it doesn’t need to be changed. However, it’s crucial to update the record every time there is a change in medication or dosage. This ensures everyone is on the same page.
- It’s only necessary for certain medications. Many assume that this form is only needed for prescription medications. The truth is, it should be used for all medications, including over-the-counter drugs and supplements. Every medication matters.
- Recording refusals is optional. Some think that if a patient refuses medication, it doesn’t need to be documented. In fact, recording refusals is essential. It helps track patient compliance and informs future care decisions.
- It’s a one-time form. Many believe that the Medication Administration Record Sheet is a one-time use form. This is incorrect. It should be used continuously for as long as the patient is receiving medications, ensuring accurate and ongoing documentation.
Common mistakes
-
Failing to include the consumer's name at the top of the form can lead to confusion. It's essential to clearly identify who is receiving the medication.
-
Not recording the attending physician's name can create issues in tracking prescriptions and understanding the medical decisions behind them.
-
Omitting the month and year can complicate record-keeping and make it difficult to reference the correct time frame for medication administration.
-
Using incorrect hour notations can lead to administering medication at the wrong time. Accuracy in timekeeping is crucial.
-
Failing to mark whether the medication was refused, discontinued, or changed can create confusion about the consumer's treatment plan.
-
Not recording the administration time can result in gaps in the medication history, making it difficult to track when medications were given.
-
Forgetting to indicate whether the consumer was in a day program or at home can affect how the medication is monitored and managed.
-
Neglecting to use clear and legible handwriting can lead to misinterpretations of the information provided on the form.
-
Failing to double-check the medication dosage can have serious implications for the consumer's health.
-
Not keeping the form updated with changes in medication can lead to discrepancies in treatment and potential health risks.
Additional PDF Templates
Dd Form 2656 March 2022 Pdf - Service members are encouraged to discuss their options before filling out the DD 2656.
Texas Odometer Disclosure Statement - The form complies with Texas regulations regarding vehicle sales.
When forming a limited liability company in Texas, it is essential to have a Texas Operating Agreement form in place, as it not only defines the operational structure but also clarifies the roles of each member. For more information and to access the necessary templates, you can visit OnlineLawDocs.com, where you will find valuable resources for Texas-based LLCs.
Return to Work Note From Doctor Pdf - Can help address any potential employment barriers early on.
Document Data
| Fact Name | Description |
|---|---|
| Purpose | The Medication Administration Record (MAR) sheet is used to document the administration of medications to consumers. |
| Consumer Identification | Each MAR sheet includes the consumer's name to ensure accurate medication administration. |
| Attending Physician | The form requires the name of the attending physician, linking medication orders to the responsible healthcare provider. |
| Monthly Tracking | The MAR is organized by month, allowing for easy tracking of medication administration over a specific period. |
| Daily Hours | It includes a grid for each hour of the day, providing a structured way to record when medications are given. |
| Refusal and Discontinuation Codes | Special codes are provided for documenting refusals (R), discontinuations (D), and changes (C) in medication. |
| Home and Day Program Indicators | The form includes indicators for home administration (H) and day program (D), ensuring clarity in the setting of medication administration. |
| Recording Requirement | It emphasizes the importance of recording the administration at the time it occurs to maintain accurate records. |
| Governing Laws | In many states, MAR sheets are governed by healthcare regulations, such as state pharmacy laws and nursing practice acts. |
Similar forms
The Medication Administration Record (MAR) is similar to a Patient Care Record. Both documents track the care provided to a patient, detailing medications administered, treatment plans, and any changes in the patient's condition. The Patient Care Record serves as a comprehensive log that healthcare providers use to ensure continuity of care and to communicate effectively with other team members. Accurate documentation in both records is crucial for patient safety and compliance with healthcare regulations.
The New York Trailer Bill of Sale form is a legal document used to record the sale and transfer of ownership of a trailer in New York State. This form captures essential details about the transaction, ensuring that both buyer and seller are protected under the law. Proper completion of this form is crucial for a smooth registration process with the Department of Motor Vehicles (DMV) and can be found at documentonline.org/blank-new-york-trailer-bill-of-sale.
Another document akin to the MAR is the Medication Log. This log specifically focuses on the administration of medications, including dosage, timing, and any reactions observed. While the MAR may include additional information about the patient’s overall care, the Medication Log emphasizes medication details. Both documents help healthcare providers monitor and manage a patient’s medication regimen effectively.
The Treatment Administration Record (TAR) shares similarities with the MAR as well. The TAR records all treatments given to a patient, including medications, therapies, and interventions. Like the MAR, it is essential for tracking what has been administered and when, ensuring that care is consistent and adheres to the prescribed treatment plan.
A Care Plan Document is also comparable to the MAR. This document outlines the overall strategy for a patient’s care, including medication management. While the MAR tracks the actual administration of medications, the Care Plan provides a broader view of the patient’s treatment goals and strategies. Both documents must align to ensure that the patient receives comprehensive and coordinated care.
The Incident Report is another relevant document. While it does not track medication administration directly, it is vital for documenting any errors or adverse reactions related to medications. The MAR may reference incidents, and both documents work together to improve patient safety and quality of care by identifying areas for improvement.
The Nursing Progress Notes are similar in that they document the ongoing observations and assessments made by nursing staff. These notes often reference medication administration and any effects observed. Both the MAR and Nursing Progress Notes are essential for ensuring that all members of the healthcare team are aware of the patient’s status and treatment history.
The Prescription Record is closely related to the MAR. This document contains details about the medications prescribed to a patient, including dosages and instructions. The MAR then tracks the administration of these prescriptions. Both documents are critical for managing a patient’s medication regimen and ensuring that all prescriptions are followed accurately.
The Discharge Summary is another document that shares similarities with the MAR. While the MAR focuses on ongoing medication administration, the Discharge Summary provides a comprehensive overview of a patient’s treatment during their stay, including medications administered. Both documents are essential for ensuring that patients receive appropriate follow-up care after discharge.
The Consent Form is also relevant. While it does not track medication administration, it ensures that patients are informed about the medications they will receive and consent to their administration. Both the MAR and Consent Form work together to uphold patient rights and ensure informed decision-making regarding treatment.
Finally, the Laboratory Results Report can be considered similar to the MAR in that it may influence medication administration decisions. This report provides critical information about a patient’s health status, which can affect medication choices. Both documents are essential for ensuring that medications are administered safely and effectively, based on the patient’s current health condition.