Blank Do Not Resuscitate Order Form
In the realm of healthcare decisions, few documents hold as much weight as the Do Not Resuscitate (DNR) Order form. This crucial legal instrument empowers individuals to express their wishes regarding medical interventions in the event of a life-threatening situation. It serves as a directive that communicates a person's desire to forgo cardiopulmonary resuscitation (CPR) and other life-saving measures, should their heart or breathing cease. The DNR Order is not merely a piece of paper; it embodies the values and preferences of the individual, ensuring that their choices are respected even when they are unable to voice them. Typically, the form requires the signature of a physician, affirming that the decision aligns with the patient's medical condition and prognosis. Additionally, it is important to understand that a DNR Order does not imply a refusal of all medical care; rather, it specifically addresses resuscitation efforts. This form can be a vital component of advance care planning, allowing individuals to engage in thoughtful discussions with their families and healthcare providers about their end-of-life wishes. Navigating the complexities of such decisions can be challenging, but the DNR Order stands as a testament to the importance of personal autonomy in healthcare choices.
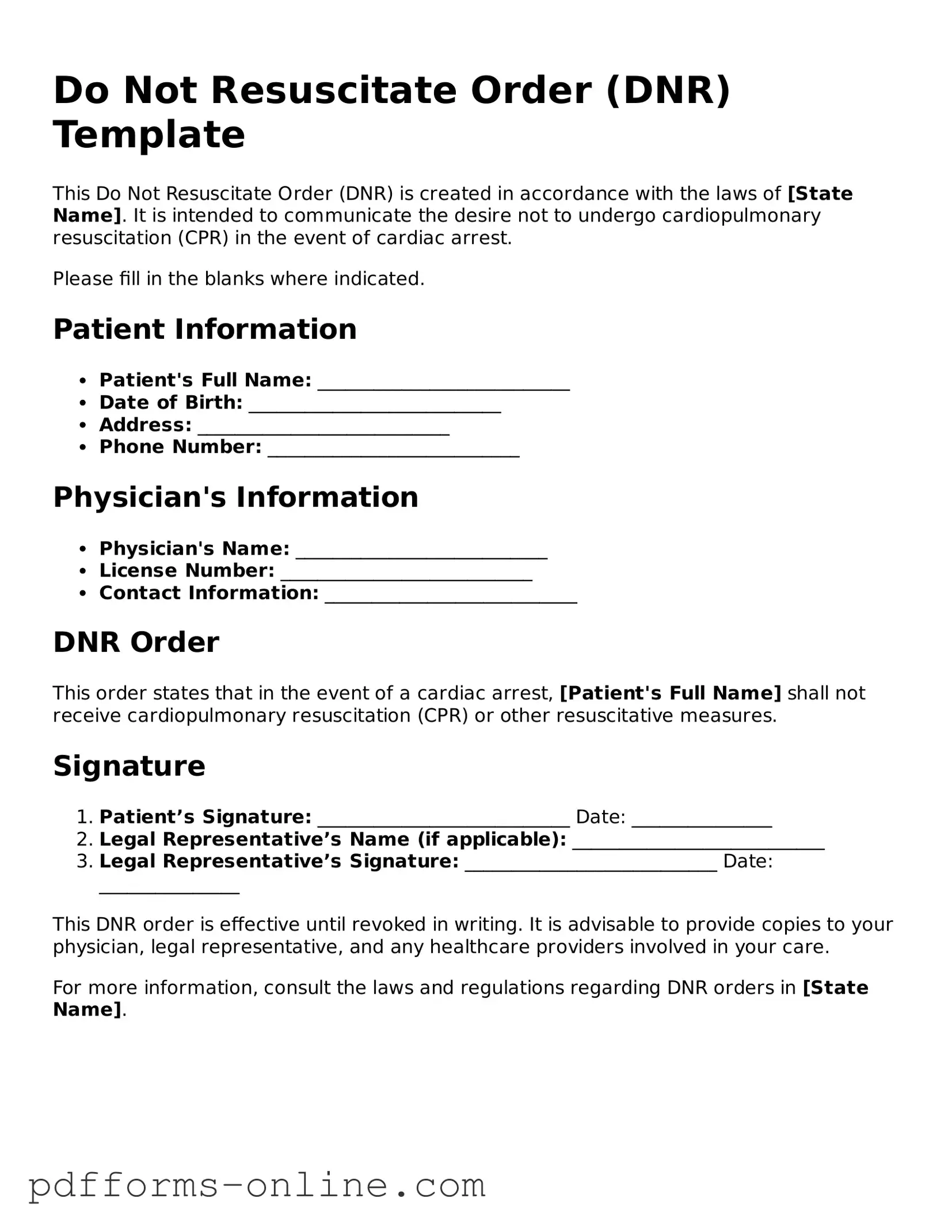
Document Example
Do Not Resuscitate Order (DNR) Template
This Do Not Resuscitate Order (DNR) is created in accordance with the laws of [State Name]. It is intended to communicate the desire not to undergo cardiopulmonary resuscitation (CPR) in the event of cardiac arrest.
Please fill in the blanks where indicated.
Patient Information
- Patient's Full Name: ___________________________
- Date of Birth: ___________________________
- Address: ___________________________
- Phone Number: ___________________________
Physician's Information
- Physician's Name: ___________________________
- License Number: ___________________________
- Contact Information: ___________________________
DNR Order
This order states that in the event of a cardiac arrest, [Patient's Full Name] shall not receive cardiopulmonary resuscitation (CPR) or other resuscitative measures.
Signature
- Patient’s Signature: ___________________________ Date: _______________
- Legal Representative’s Name (if applicable): ___________________________
- Legal Representative’s Signature: ___________________________ Date: _______________
This DNR order is effective until revoked in writing. It is advisable to provide copies to your physician, legal representative, and any healthcare providers involved in your care.
For more information, consult the laws and regulations regarding DNR orders in [State Name].
State-specific Guides for Do Not Resuscitate Order Documents
Frequently Asked Questions
-
What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order, often referred to as a DNR, is a legal document that informs medical professionals not to perform cardiopulmonary resuscitation (CPR) if a patient’s heart stops beating or if they stop breathing. This decision is typically made by the patient or their legal representative when they wish to avoid aggressive medical interventions in the event of a life-threatening situation.
-
Who should consider having a DNR Order?
Individuals who have serious health conditions, are facing terminal illnesses, or those who have specific wishes regarding end-of-life care may want to consider a DNR Order. It is particularly important for patients who prefer to die naturally rather than undergo invasive procedures that may not improve their quality of life. Discussing these wishes with family members and healthcare providers can help ensure that everyone is on the same page.
-
How do I obtain a DNR Order?
To obtain a DNR Order, you typically need to have a conversation with your healthcare provider. They will provide the necessary forms and guide you through the process. In many states, a DNR must be signed by a physician and may require the signature of the patient or their legal representative. It’s essential to keep copies of the signed order in accessible locations, such as with your medical records or at home, to ensure that emergency personnel can easily find it.
-
Can a DNR Order be changed or revoked?
Yes, a DNR Order can be changed or revoked at any time. If a patient’s wishes change or if their health status improves, they can inform their healthcare provider to update or cancel the order. It is important to communicate any changes clearly and to ensure that all copies of the DNR are updated accordingly. Keeping family members informed about these changes is also crucial to avoid confusion during emergencies.
Misconceptions
Understanding the Do Not Resuscitate (DNR) Order form is crucial for patients and their families. Here are ten common misconceptions about DNR orders:
- A DNR means no medical care at all. This is false. A DNR only specifies that a person does not want resuscitation efforts in the event of cardiac arrest. Other medical treatments may still be provided.
- DNR orders are only for terminally ill patients. Not true. While many people with terminal illnesses have DNR orders, anyone can choose to have one, regardless of their health status.
- A DNR is the same as a living will. This is incorrect. A living will outlines a person's wishes regarding medical treatment in various situations, while a DNR specifically addresses resuscitation efforts.
- Once a DNR is signed, it cannot be changed. This is a misconception. A DNR can be revoked or modified at any time by the patient or their legal representative.
- DNR orders are only valid in hospitals. This is misleading. DNR orders can be valid in various settings, including at home and in long-term care facilities, depending on state laws.
- All medical staff know about my DNR order. This is not always the case. It is essential to ensure that your DNR order is documented in your medical records and communicated to all relevant healthcare providers.
- DNR orders are legally binding in all states. This is inaccurate. The legality and recognition of DNR orders can vary by state, so it is important to understand local laws.
- A DNR order means I will die sooner. This is a misconception. A DNR order does not hasten death; it simply respects the patient's wishes regarding resuscitation efforts.
- Family members can override a DNR order. This is generally false. A DNR order is a legal document, and family members typically cannot override it unless they have legal authority, such as being a designated healthcare proxy.
- Having a DNR order means I cannot receive other treatments. This is incorrect. Patients with DNR orders can still receive other forms of medical treatment, such as pain management and comfort care.
Clearing up these misconceptions can help individuals make informed decisions about their healthcare preferences.
Common mistakes
-
Failing to discuss the decision with family members. Open conversations can prevent confusion and ensure everyone understands the patient's wishes.
-
Not consulting with a healthcare provider. Medical professionals can provide essential guidance on the implications of a Do Not Resuscitate (DNR) order.
-
Leaving the form unsigned. An unsigned form is not legally binding and may lead to unwanted resuscitation efforts.
-
Using outdated forms. Ensure the DNR order is the most current version, as regulations can change over time.
-
Not specifying the scope of the order. A DNR should clearly state whether it applies only to resuscitation efforts or extends to other medical interventions.
-
Neglecting to keep copies accessible. A DNR order should be easily accessible to healthcare providers and family members in case of an emergency.
-
Failing to update the order when circumstances change. Life events, health status, or personal wishes may necessitate a revision of the DNR order.
-
Not communicating the existence of the DNR order to emergency responders. Informing all relevant parties ensures that the order is honored.
-
Overlooking state-specific requirements. Each state may have unique laws governing DNR orders, and compliance is crucial.
-
Assuming verbal agreements are sufficient. Written documentation is essential for legal recognition of the DNR order.
Popular Templates
Free Printable Puppy Health Guarantee Template - A necropsy is required if the puppy dies to determine the cause.
Minor Car Accident Settlement Letter - It serves to confirm that repairs and compensation are resolved.
The Arizona Independent Contractor Agreement serves as an essential legal document for businesses engaging with independent contractors, detailing the terms of work, payment, and responsibilities. By providing clear guidelines, it helps to prevent misunderstandings and disputes between both parties, fostering a professional working relationship. For those looking to formalize such an arrangement, you can access the Independent Contractor Agreement form to ensure all necessary details are captured.
Affixture - This form helps in updating title records to reflect the correct status of the property.
PDF Attributes
| Fact Name | Details |
|---|---|
| Definition | A Do Not Resuscitate (DNR) order is a legal document that indicates a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. |
| Purpose | The primary purpose of a DNR order is to respect the wishes of individuals who do not want life-sustaining treatment in certain medical situations. |
| Legal Status | DNR orders are legally recognized documents in all 50 states, though specific requirements may vary by state. |
| State-Specific Forms | Many states have their own specific DNR forms, which must be completed and signed according to state laws. |
| Governing Laws | In California, for example, the DNR order is governed by the California Health and Safety Code, Section 7180. |
| Signature Requirement | A DNR order typically requires the signature of the patient or their legal representative, along with a physician's signature. |
| Revocation | Individuals can revoke a DNR order at any time, either verbally or in writing, and should inform their healthcare providers of the change. |
| Emergency Medical Services | Emergency medical personnel are required to follow DNR orders, provided they are valid and properly executed. |
| Communication | It is essential to communicate the existence of a DNR order to family members and healthcare providers to ensure compliance with the individual's wishes. |
| Advance Directives | A DNR order can be part of a broader advance directive, which outlines an individual's healthcare preferences in various situations. |
Similar forms
A Living Will is a document that outlines an individual's preferences for medical treatment in situations where they are unable to communicate their wishes. Like a Do Not Resuscitate Order (DNR), it provides guidance to healthcare providers regarding the patient’s desires, particularly concerning end-of-life care. Both documents focus on the patient’s autonomy and ensure that their choices are respected in critical situations.
A Healthcare Power of Attorney grants a designated person the authority to make medical decisions on behalf of another individual if they become incapacitated. Similar to a DNR, this document emphasizes the importance of patient preferences. It allows individuals to choose someone they trust to advocate for their medical wishes, ensuring that their healthcare aligns with their values and desires.
An Advance Directive combines elements of both a Living Will and a Healthcare Power of Attorney. This document allows individuals to specify their medical treatment preferences while also appointing an agent to make decisions on their behalf. Like a DNR, it serves to communicate the patient's wishes, ensuring that healthcare providers understand their choices regarding life-sustaining treatments.
A Physician Orders for Life-Sustaining Treatment (POLST) form is designed for individuals with serious health conditions. It translates patient preferences into actionable medical orders. Similar to a DNR, a POLST form provides clear instructions to healthcare providers about the patient’s wishes regarding resuscitation and other life-sustaining measures, ensuring that those preferences are honored in emergency situations.
An organ donation consent form allows individuals to express their wishes regarding organ donation after death. While not directly related to resuscitation, it reflects the individual’s choices about their body after passing. Both documents highlight the importance of honoring a person's wishes and ensuring that their preferences are respected in critical situations.
A Mental Health Advance Directive allows individuals to outline their preferences for mental health treatment in case they become unable to make decisions. This document is similar to a DNR in that it empowers individuals to communicate their wishes regarding treatment, ensuring that their rights and preferences are upheld, especially during times of crisis.
A Do Not Intubate (DNI) order specifies that a patient does not wish to be placed on a ventilator in the event of respiratory failure. Like a DNR, a DNI order is a critical part of advance care planning. Both documents serve to communicate the patient’s preferences for life-sustaining measures and protect their autonomy in medical decision-making.
A Palliative Care Plan outlines the goals and preferences for care focused on providing relief from symptoms of serious illness. This document is similar to a DNR in that it prioritizes the comfort and quality of life for the patient. Both emphasize the importance of aligning medical interventions with the patient’s values and desires, particularly in the face of terminal conditions.
For those involved in the mobile home transaction process, understanding the necessary documentation is essential. Accurate completion of forms not only facilitates a smooth sale but also helps to avoid potential disputes later on. This is particularly true for the Mobile Home Bill of Sale, which is crucial for ensuring clarity between parties. To explore additional documentation that may be needed, refer to All Arizona Forms for a comprehensive list of resources.
A Do Not Hospitalize (DNH) order indicates that a patient does not wish to be admitted to a hospital for treatment. This document shares similarities with a DNR as both express the patient's wishes regarding the type of medical care they wish to receive. Both documents ensure that healthcare providers respect the patient's choices in critical situations.
A Medical Order for Scope of Treatment (MOST) form is used in some states to outline a patient’s preferences for various types of medical treatment. Similar to a DNR, this form provides specific instructions to healthcare providers regarding the patient’s wishes. Both documents serve to ensure that the individual’s choices regarding their healthcare are clearly communicated and honored during emergencies.