Valid California Do Not Resuscitate Order Template
In California, the Do Not Resuscitate (DNR) Order form is an important legal document that allows individuals to express their wishes regarding medical treatment in the event of a life-threatening situation. This form is particularly significant for those who prefer not to receive cardiopulmonary resuscitation (CPR) or other life-saving measures if their heart stops or they stop breathing. It is designed to ensure that healthcare providers respect the patient's preferences during critical moments. The DNR Order must be completed and signed by the patient or their legally authorized representative, and it requires a physician's signature to be valid. By understanding the key components of this form, including who can initiate it and how it can be revoked, individuals can make informed decisions that align with their values and medical care preferences. Additionally, it's essential to keep the DNR Order accessible to healthcare providers and family members to avoid confusion in emergencies. Knowing the ins and outs of the DNR Order can provide peace of mind, ensuring that one's healthcare wishes are honored when it matters most.
Document Example
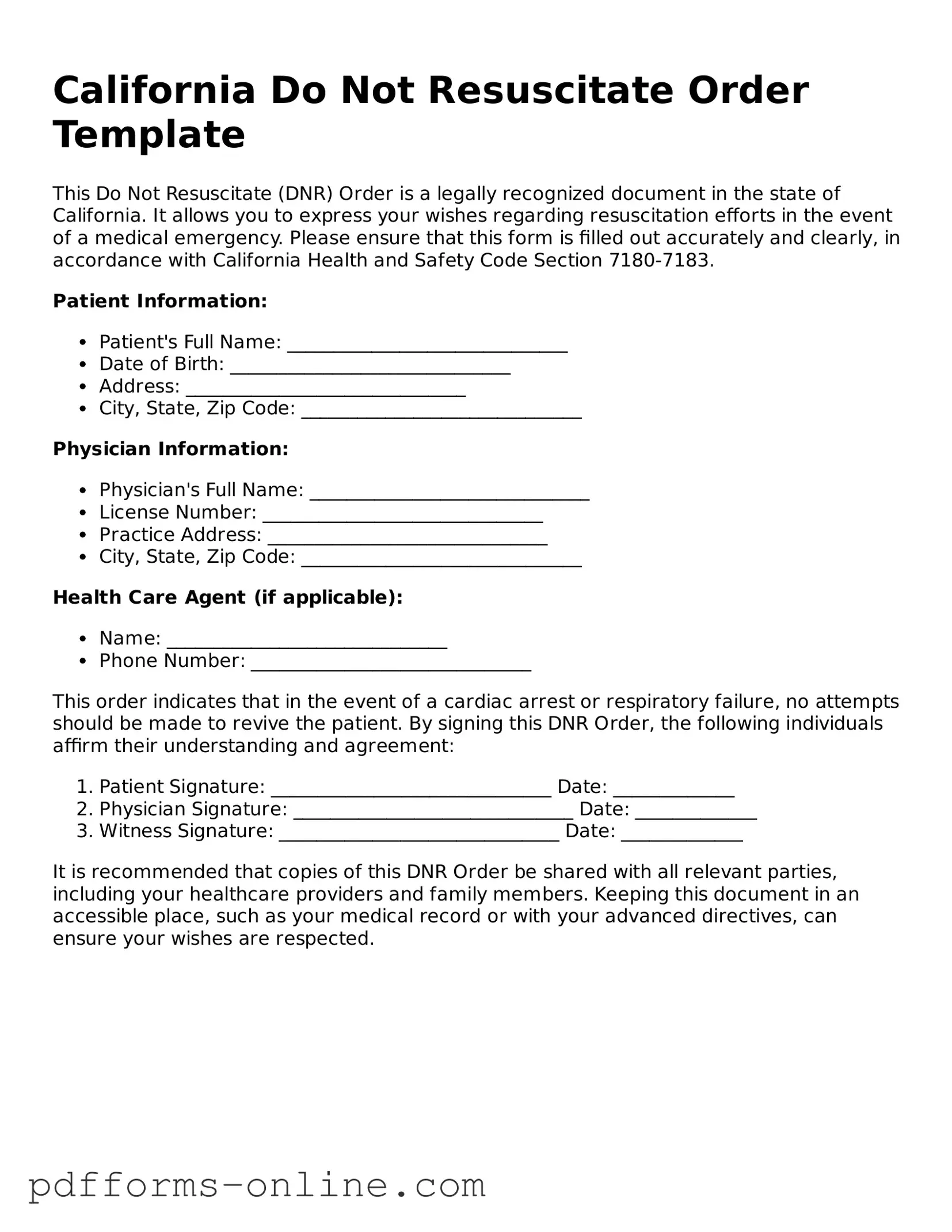
California Do Not Resuscitate Order Template
This Do Not Resuscitate (DNR) Order is a legally recognized document in the state of California. It allows you to express your wishes regarding resuscitation efforts in the event of a medical emergency. Please ensure that this form is filled out accurately and clearly, in accordance with California Health and Safety Code Section 7180-7183.
Patient Information:
- Patient's Full Name: ______________________________
- Date of Birth: ______________________________
- Address: ______________________________
- City, State, Zip Code: ______________________________
Physician Information:
- Physician's Full Name: ______________________________
- License Number: ______________________________
- Practice Address: ______________________________
- City, State, Zip Code: ______________________________
Health Care Agent (if applicable):
- Name: ______________________________
- Phone Number: ______________________________
This order indicates that in the event of a cardiac arrest or respiratory failure, no attempts should be made to revive the patient. By signing this DNR Order, the following individuals affirm their understanding and agreement:
- Patient Signature: ______________________________ Date: _____________
- Physician Signature: ______________________________ Date: _____________
- Witness Signature: ______________________________ Date: _____________
It is recommended that copies of this DNR Order be shared with all relevant parties, including your healthcare providers and family members. Keeping this document in an accessible place, such as your medical record or with your advanced directives, can ensure your wishes are respected.
Frequently Asked Questions
-
What is a Do Not Resuscitate (DNR) Order in California?
A Do Not Resuscitate Order is a medical order that instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a patient stops breathing or their heart stops beating. In California, this order is typically indicated by a specific form that must be filled out and signed by a physician.
-
Who can request a DNR Order?
Any adult patient who is capable of making their own healthcare decisions can request a DNR Order. Additionally, a legally authorized representative, such as a family member or a designated healthcare proxy, can request this order on behalf of an incapacitated patient.
-
How is a DNR Order created in California?
To create a DNR Order, a patient or their representative must complete the California DNR form. This form requires the patient's information, a statement of their wishes regarding resuscitation, and the signature of a physician. Once completed, the form should be kept in an easily accessible location, such as with the patient’s medical records or at home.
-
Is a DNR Order legally binding?
Yes, a properly executed DNR Order is legally binding in California. Healthcare providers are required to honor the wishes outlined in the order. However, it is essential for the order to be signed by a physician and for the patient or their representative to have a copy readily available.
-
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time. The patient or their representative can verbally communicate their wish to revoke the order, or they can destroy the existing DNR form. It is advisable to inform healthcare providers of the revocation to ensure that they are aware of the updated wishes.
-
Where should a DNR Order be kept?
A DNR Order should be kept in a location that is easily accessible to both the patient and healthcare providers. Common places include the patient’s medical records, at home in a visible location, or with other important documents. It is also helpful to inform family members and caregivers about the order’s location.
-
What happens if a DNR Order is not available during a medical emergency?
If a DNR Order is not available during a medical emergency, healthcare providers are obligated to perform CPR and other life-saving measures. It is crucial for patients and their families to ensure that the DNR Order is accessible and communicated to all relevant parties to prevent unwanted resuscitation efforts.
Misconceptions
Many people have misunderstandings about the California Do Not Resuscitate (DNR) Order form. Clarifying these misconceptions can help individuals make informed decisions about their healthcare preferences. Here are six common misconceptions:
-
A DNR means that I will not receive any medical care.
This is not true. A DNR specifically instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. You will still receive other forms of medical treatment and care.
-
A DNR can be requested by anyone, regardless of their health status. It is a personal choice based on individual values and preferences about end-of-life care.
-
This is a misconception. A DNR can be revoked or modified at any time by the individual or their legally authorized representative.
-
While legal advice can be helpful, it is not required to fill out a DNR form. The form is designed to be straightforward and can be completed by individuals without legal assistance.
-
Your DNR decision is personal. While discussing your wishes with family is encouraged, ultimately, the choice is yours to make.
-
This is a common misconception. People of all ages can have a DNR order if they wish to refuse resuscitation in the event of cardiac arrest.
Understanding these points can empower you to make decisions that align with your healthcare wishes. Always consult with a healthcare provider to discuss any concerns or questions regarding DNR orders.
Common mistakes
-
Not Understanding the Purpose: Many individuals mistakenly fill out the Do Not Resuscitate (DNR) Order form without fully grasping its implications. A DNR order is a medical directive that indicates a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. Without a clear understanding, individuals may inadvertently choose a DNR when they actually desire all possible medical interventions.
-
Inadequate Communication with Healthcare Providers: Failing to discuss the DNR order with doctors or healthcare professionals can lead to confusion and misinterpretation of one's wishes. It's crucial to have open conversations with medical teams, ensuring they understand the reasons behind the decision and the individual's overall healthcare goals.
-
Not Including Required Signatures: A common oversight is neglecting to obtain the necessary signatures on the DNR form. In California, the form must be signed by the individual or their legally authorized representative, as well as a witness. Omitting these signatures can render the document invalid, leaving healthcare providers uncertain about the patient’s wishes.
-
Forgetting to Update the Form: Life circumstances change, and so can a person's wishes regarding resuscitation. Failing to revisit and update the DNR order after significant life events—such as a serious illness, change in health status, or shifts in personal beliefs—can lead to situations where the DNR may no longer reflect the individual's current desires.
Find Some Other Do Not Resuscitate Order Forms for Specific States
How Do You Get a Dnr - Some states require a witness to sign the DNR form as well.
Dnr Form Nc - Healthcare providers are obligated to honor a valid DNR order as part of their duty to respect patient autonomy.
When considering a Power of Attorney form in Texas, it's crucial to understand that this document not only allows someone to make decisions for you in times of need but also ensures that your wishes are respected. For those looking to obtain or learn more about this important legal tool, resources such as OnlineLawDocs.com can provide valuable guidance and information.
Illinois Do Not Resuscitate - Having a Do Not Resuscitate Order can promote peace for both patients and their loved ones.
Georgia Do Not Resuscitate Form - A DNR order is part of the continuum of care provided to individuals facing serious health challenges.
PDF Attributes
| Fact Name | Description |
|---|---|
| Purpose | The California Do Not Resuscitate (DNR) Order form allows individuals to refuse cardiopulmonary resuscitation (CPR) in the event of a medical emergency. |
| Governing Law | The DNR Order in California is governed by California Health and Safety Code Section 7180-7190. |
| Eligibility | Any adult may complete a DNR Order. Minors require consent from a parent or legal guardian. |
| Signature Requirement | The form must be signed by the individual or their authorized representative, along with a physician’s signature. |
| Form Availability | The DNR Order form is available through healthcare providers, hospitals, and online resources. |
| Revocation | Individuals can revoke a DNR Order at any time. This can be done verbally or by destroying the form. |
| Emergency Services | Emergency medical personnel are required to honor a valid DNR Order in the field. |
| Notification | It is crucial to inform family members and healthcare providers about the existence of a DNR Order. |
| Storage | The DNR Order should be kept in an easily accessible location, such as a medical file or on the refrigerator. |
Similar forms
The Advance Healthcare Directive is a crucial document that allows individuals to outline their healthcare preferences in advance. Similar to the California Do Not Resuscitate Order (DNR), it enables people to express their wishes regarding medical treatment if they become unable to communicate. This directive can include preferences about life-sustaining treatments, organ donation, and appointing a healthcare agent to make decisions on their behalf. Both documents serve to ensure that a person's healthcare choices are respected, even when they cannot voice them directly.
The Physician Orders for Life-Sustaining Treatment (POLST) form is another important document that shares similarities with the DNR. POLST is designed for individuals with serious health conditions and translates their treatment preferences into actionable medical orders. Like the DNR, it specifically addresses the use of resuscitation and other life-sustaining measures. The POLST form is intended to be more detailed than a DNR, often including preferences about various treatments, making it a valuable tool for emergency responders and healthcare providers.
The Living Will is a document that allows individuals to specify their preferences for medical treatment in the event they become incapacitated. Similar to a DNR, a Living Will communicates the types of medical interventions a person does or does not want. While the DNR focuses specifically on resuscitation efforts, the Living Will encompasses a broader range of medical decisions. Both documents aim to provide clarity and ensure that healthcare providers honor the patient's wishes.
The Healthcare Proxy is a legal document that designates someone to make healthcare decisions on behalf of an individual if they are unable to do so. Like the DNR, it emphasizes the importance of respecting a person's wishes regarding medical treatment. While the DNR provides specific instructions about resuscitation, the Healthcare Proxy empowers a trusted individual to interpret and act upon the patient's broader healthcare preferences. This relationship can be crucial in ensuring that the person’s values and desires are upheld during medical crises.
The Do Not Intubate (DNI) order is another document that is closely related to the DNR. A DNI order specifically instructs healthcare providers not to place a patient on a ventilator if they are unable to breathe on their own. This document complements the DNR by providing clarity on the patient's wishes regarding mechanical ventilation. Both documents reflect a patient’s desire to avoid aggressive life-sustaining treatments and focus on comfort and quality of life.
The Medical Power of Attorney (MPOA) grants an individual the authority to make medical decisions on behalf of another person. Like the DNR, it ensures that a person's healthcare preferences are respected. The MPOA can cover a wide range of medical decisions, while the DNR specifically addresses resuscitation. Both documents work together to provide a comprehensive approach to healthcare decision-making, ensuring that a patient's wishes are honored, even in challenging situations.
The Comfort Care Order is a document that outlines a patient's desire for comfort-focused care rather than aggressive treatment. Similar to the DNR, it emphasizes the importance of prioritizing the patient's quality of life. The Comfort Care Order specifies that, in the event of a medical emergency, the focus should be on alleviating pain and discomfort rather than prolonging life through invasive procedures. Both documents reflect a compassionate approach to end-of-life care.
The New York Trailer Bill of Sale form is an essential legal document that facilitates the sale and transfer of trailer ownership within New York State. To avoid any ambiguities during this process, it is important for both buyers and sellers to be well-informed about the details outlined in this document, as it protects the rights of both parties involved. For more information about this form, you can visit https://documentonline.org/blank-new-york-trailer-bill-of-sale, which provides comprehensive insights into its usage and significance.
The Do Not Hospitalize (DNH) order is a document that expresses a patient’s preference to avoid hospitalization in certain circumstances. Like the DNR, it aims to honor the patient's wishes regarding medical interventions. The DNH order can be particularly important for individuals with terminal illnesses or advanced chronic conditions who wish to remain in a familiar environment, such as their home or a hospice setting. Both documents advocate for a patient-centered approach to healthcare decisions, ensuring that individuals receive the type of care they desire.