Blank Annual Physical Examination Template
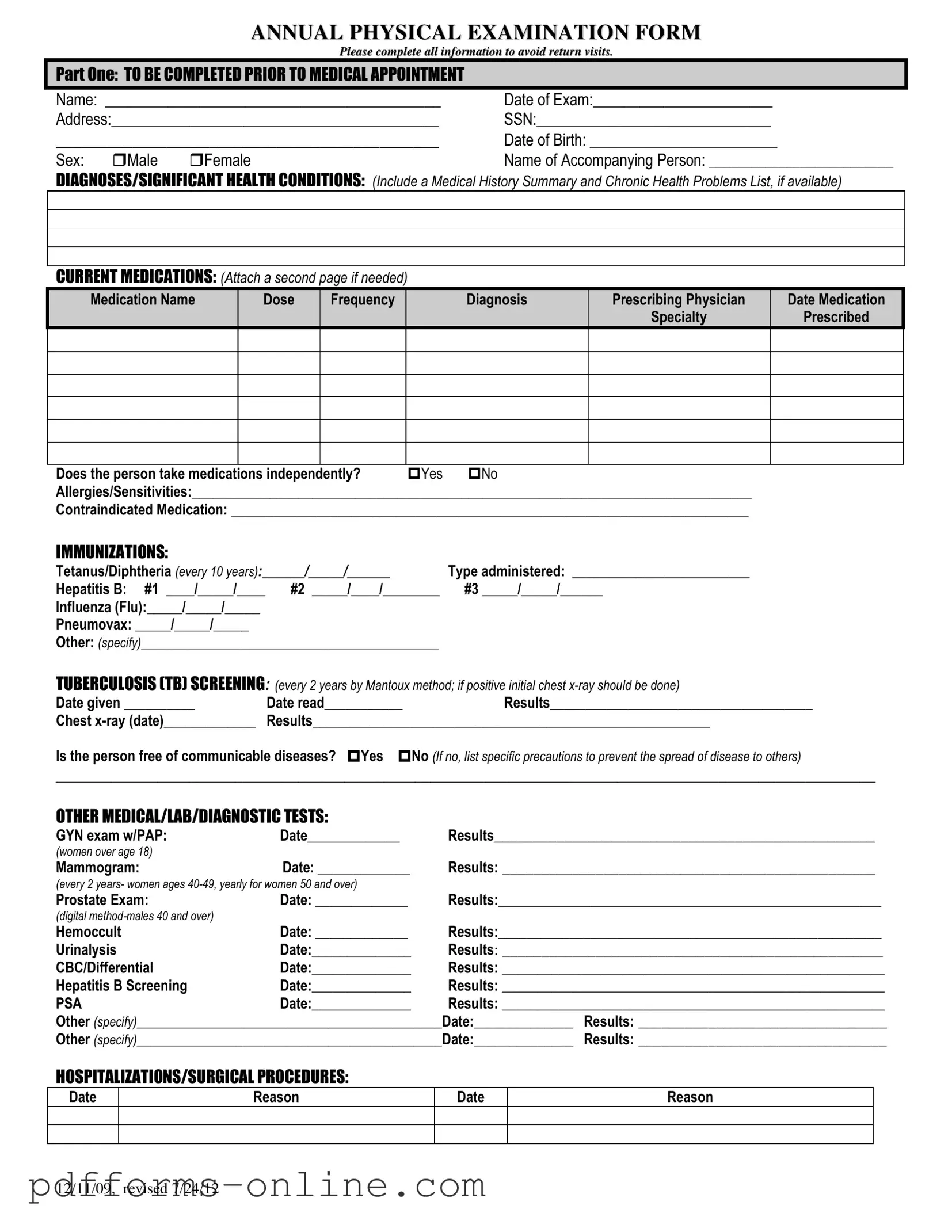
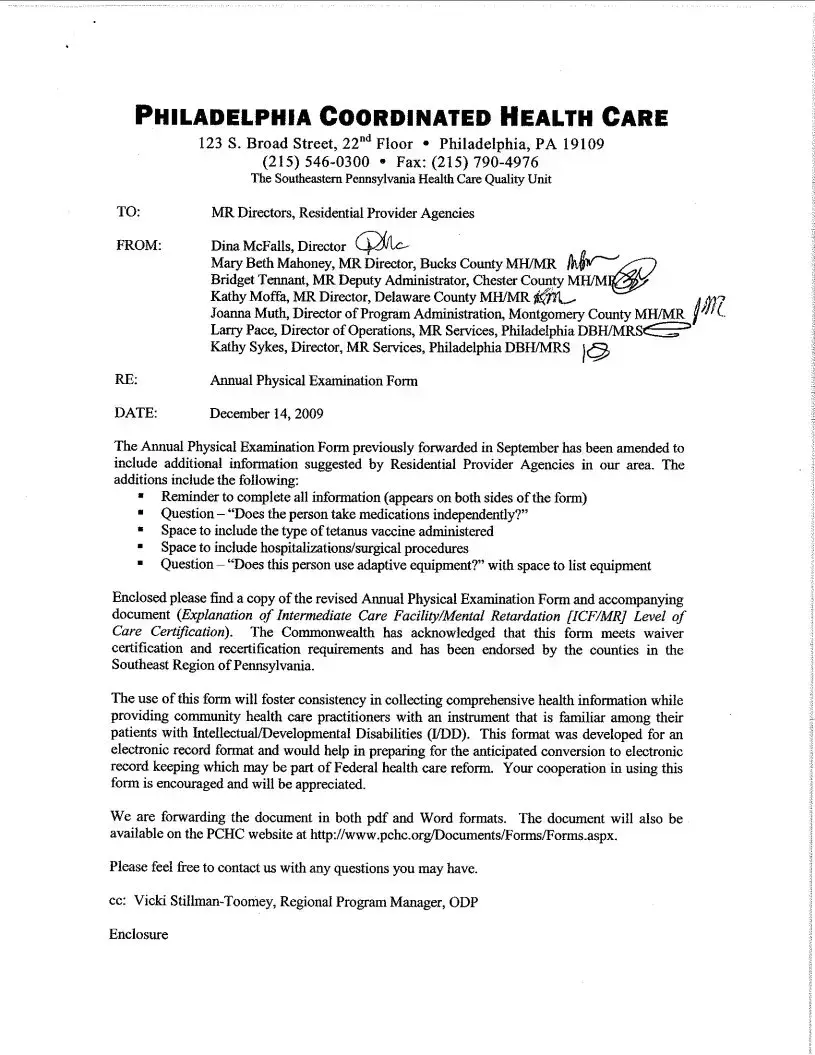
The Annual Physical Examination form serves as a crucial tool for gathering comprehensive health information prior to a medical appointment. It is divided into two main sections, each designed to capture essential details about an individual’s medical history and current health status. The first part requires the completion of personal information, including name, date of birth, and social security number, along with a summary of significant health conditions and current medications. This section also addresses allergies, immunizations, and any past hospitalizations or surgical procedures. The second part focuses on the general physical examination, where basic vitals such as blood pressure, pulse, and weight are recorded. Additionally, a systematic evaluation of various body systems is conducted, allowing healthcare providers to note normal findings or any concerns. Recommendations for health maintenance, dietary considerations, and any necessary follow-up tests or specialist referrals are also included. This structured approach aims to ensure that all relevant health information is collected, ultimately facilitating a more effective and informed medical evaluation.
Document Example
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Frequently Asked Questions
-
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect important health information before your medical appointment. It helps healthcare providers understand your medical history, current medications, allergies, and any significant health conditions. Completing this form accurately ensures a more efficient and effective visit.
-
What information do I need to provide on the form?
You will need to fill out your personal details, including your name, date of birth, and address. Additionally, you should list any significant health conditions, current medications, allergies, and immunizations. If applicable, include information about previous hospitalizations or surgeries. This comprehensive information helps your doctor assess your health accurately.
-
How often should I complete this form?
The Annual Physical Examination form should be completed every year prior to your physical examination. This annual update allows your healthcare provider to track any changes in your health and adjust your care accordingly. If you have new medications or health issues, it’s important to note these changes each year.
-
What if I don't have all the information requested?
If you don’t have certain information, such as past medical records or specific medication details, it’s okay to leave those sections blank. However, try to provide as much information as possible. You can also bring any relevant documents to your appointment to help fill in the gaps.
-
What should I do if I have questions about the form?
If you have questions while filling out the form, don’t hesitate to ask your healthcare provider for assistance. They can help clarify any sections you find confusing. It’s important that the form is completed accurately, so feel free to seek guidance if needed.
Misconceptions
Misconceptions about the Annual Physical Examination form can lead to confusion and missed opportunities for health management. Here are ten common misconceptions:
- It’s only for sick people. Many believe that annual physicals are only necessary if someone is feeling unwell. In reality, these exams are crucial for preventive care and identifying potential health issues early.
- All information is optional. Some people think they can skip sections of the form. Completing all sections is essential to provide a comprehensive view of health, which helps the physician make informed decisions.
- Medications don’t need to be listed if they are over-the-counter. Even over-the-counter medications can interact with prescribed treatments. It’s important to list all medications, regardless of their type.
- Immunization records are not necessary. Some individuals may assume that they do not need to provide immunization history. However, this information is vital for assessing health risks and ensuring appropriate vaccinations are up to date.
- Only adults need physical exams. There’s a misconception that only adults require annual physicals. Children and adolescents also benefit from regular check-ups to monitor their growth and development.
- Results from previous years are irrelevant. Many people overlook the importance of past medical history. Previous results can provide valuable context for current health assessments and trends.
- Physical exams are the same every year. Each examination can vary based on age, medical history, and current health conditions. The form is tailored to gather specific information relevant to each individual.
- You can fill out the form during the appointment. Some believe they can complete the form in the waiting room. It’s best to fill it out beforehand to ensure all information is accurate and complete.
- There’s no need for a follow-up if nothing seems wrong. Even if no immediate issues are detected, follow-up appointments may be necessary to monitor ongoing health or changes over time.
- Only doctors review the form. While physicians ultimately assess the information, nurses and other healthcare professionals also rely on the details provided to offer comprehensive care.
Common mistakes
-
Incomplete Personal Information: Failing to fill out all personal details, such as name, date of birth, or address, can lead to delays in processing. Ensure every section is complete to avoid return visits.
-
Neglecting Medication Details: Omitting current medications or not providing accurate dosage and frequency can impact the evaluation. Always list all medications, including over-the-counter drugs and supplements.
-
Ignoring Allergies: Not mentioning allergies or sensitivities can pose serious risks during examinations. It is crucial to disclose any known allergies to prevent adverse reactions.
-
Overlooking Immunization Records: Failing to provide accurate immunization dates can lead to complications. Ensure all immunizations are listed, including the type and dates administered.
-
Inaccurate Medical History: Providing incomplete or incorrect medical history can mislead healthcare providers. Be thorough and honest about past surgeries, hospitalizations, and chronic conditions.
-
Forgetting Follow-Up Recommendations: Not noting any recommendations for further evaluations or tests can result in missed health checks. Pay attention to any suggested follow-ups from the physician.
Additional PDF Templates
Signing Over Parental Rights in Sc - Legal advice may be beneficial when completing the affidavit.
The New York Mobile Home Bill of Sale form is not only essential for streamlining ownership transfer but can also be accessed and downloaded for your convenience at https://documentonline.org/blank-new-york-mobile-home-bill-of-sale/. This document ensures that both the buyer and seller maintain a clear record of the transaction, providing critical details about the mobile home and its sale, thereby enhancing transparency and peace of mind for everyone involved.
Uscis Forms - Attach evidence of assets if income is not enough to meet the requirements.
Document Data
| Fact Name | Description |
|---|---|
| Purpose | The Annual Physical Examination form is designed to collect comprehensive health information prior to a medical appointment. |
| Patient Information | Patients must provide personal details such as name, date of birth, and Social Security Number to ensure accurate medical records. |
| Medication Disclosure | Current medications must be listed, including dosage and prescribing physician, to inform the medical provider of any potential interactions. |
| Immunization Records | Patients are required to document their immunization history, including dates for vaccines like Tetanus and Hepatitis B. |
| Health Conditions | Individuals must disclose any significant health conditions or allergies to ensure safe and effective medical care. |
| Legal Compliance | In many states, the collection of this information is governed by health privacy laws, such as HIPAA, which protect patient information. |
| Follow-Up Actions | The form may prompt further evaluations or tests based on the findings during the physical examination, ensuring ongoing patient care. |
Similar forms
The Annual Physical Examination form shares similarities with the Health History Questionnaire. Both documents collect essential personal information, including the individual's name, date of birth, and medical history. The Health History Questionnaire typically focuses on past illnesses, surgeries, and family medical history, which helps healthcare providers understand a patient’s background. Like the Annual Physical Examination form, it aims to create a comprehensive picture of the patient's health to guide future medical care and decisions.
A Residential Lease Agreement form is a vital document that outlines the understanding between a landlord and a tenant regarding the rental of residential property. It serves as a legally binding contract that details the rights and responsibilities of each party. This form is the foundation for ensuring a clear, fair, and enforceable arrangement for both landlords and tenants, which can easily be accessed at OnlineLawDocs.com.
Another document akin to the Annual Physical Examination form is the Medication Reconciliation Form. This form is used to list all current medications a patient is taking, including dosages and frequencies. Just as the Annual Physical Examination form requires detailed information about medications, the Medication Reconciliation Form ensures that healthcare providers have an accurate understanding of a patient's medication regimen. This helps prevent potential drug interactions and ensures continuity of care during medical appointments.
The Immunization Record is also similar to the Annual Physical Examination form in that it tracks vaccinations a patient has received. Both documents require specific dates and types of immunizations, which are crucial for maintaining public health and individual well-being. The Immunization Record provides a clear overview of a patient's vaccination history, while the Annual Physical Examination form may include this information as part of a broader health assessment.
Lastly, the Patient Intake Form bears resemblance to the Annual Physical Examination form. It gathers demographic information and medical history before a patient’s appointment. Both forms aim to streamline the patient experience by collecting vital information upfront. The Patient Intake Form often includes questions about lifestyle habits and allergies, similar to the Annual Physical Examination form’s focus on current medications and allergies, ensuring that healthcare providers have the necessary context to deliver effective care.